How to Manage Interactions When Starting a New Medication

Starting a new medication can be simple - pick up the prescription, read the label, take it as directed. But what if that new pill doesn’t just work on its own? What if it teams up with something else you’re taking - a blood pressure drug, a supplement, even grapefruit juice - and turns dangerous?
Drug interactions aren’t rare. They happen every day. In fact, drug interactions are behind nearly one in five medication errors in the U.S., according to the Institute for Safe Medication Practices. And for people over 65 taking five or more medications? The risk jumps to 30%. That’s not a small chance. That’s a real, avoidable danger.
What Exactly Is a Drug Interaction?
A drug interaction happens when one medication changes how another one works in your body. This isn’t about allergies or side effects you’ve never seen before. It’s about chemistry - how your body absorbs, breaks down, or responds to drugs when they’re mixed.
There are two main types:
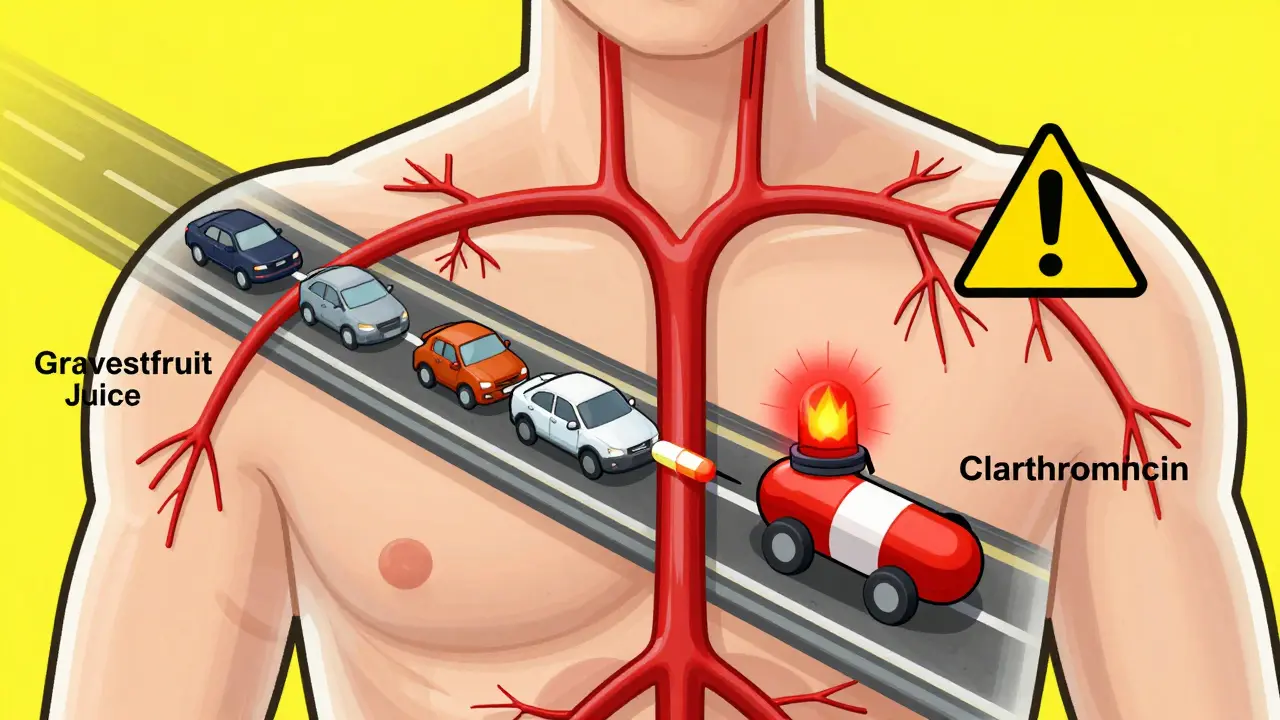
- Pharmacokinetic interactions - These affect how your body moves the drug around. Think of it like traffic on a highway. One drug might slow down or block the road, so another drug builds up to dangerous levels. The most common culprit? The CYP3A4 enzyme. It handles about half of all prescription drugs. When something like clarithromycin or grapefruit juice blocks it, levels of drugs like simvastatin or cyclosporine can spike 3x or more.
- Pharmacodynamic interactions - These happen when two drugs amplify each other’s effects. Take blood thinners. If you start taking a new anticoagulant like apixaban while still on low-molecular-weight heparin, your bleeding risk doesn’t just go up a little. It jumps 300-400%. Or consider opioids and promethazine. Together, they can crush your breathing - a combo that’s led to preventable deaths.
Top 5 High-Risk Interactions You Need to Know
Not all interactions are created equal. Some are mild. Others are life-threatening. Here are five that come up again and again in clinics:
- Simvastatin + Amlodipine or Diltiazem - Statins lower cholesterol. Calcium channel blockers like amlodipine treat high blood pressure. But together? Simvastatin can build up to toxic levels. The fix? Cap simvastatin at 20 mg/day with amlodipine. With diltiazem or verapamil? Drop it to 10 mg. Many patients don’t know this. Pharmacist-led reviews cut these errors by 40%.
- Warfarin + Amiodarone - Amiodarone, used for irregular heartbeat, can double warfarin’s effect. The result? A spike in INR levels. Without adjustment, bleeding risk skyrockets. The standard: cut warfarin dose by 30-50% right away, then check INR within 3-5 days.
- MAO Inhibitors + Aged Cheese - MAOIs like phenelzine are antidepressants. But they can’t touch foods with tyramine - aged cheeses, cured meats, draft beer. One serving of cheddar (2-5 mg tyramine) can trigger a hypertensive crisis. Blood pressure can surge past 200 mmHg. This isn’t theoretical. It’s happened in ERs.
- St. John’s Wort + Antidepressants or Birth Control - This herbal supplement is popular for mood. But it speeds up liver enzymes, making drugs like sertraline or birth control pills useless. Studies show it can slash cyclosporine levels by 60%. And 68% of patients never tell their doctor they’re taking it.
- Opioids + Benzodiazepines or Antihistamines - Mixing opioids with sedatives like lorazepam or diphenhydramine? That’s a one-way ticket to respiratory depression. The FDA has issued black box warnings. Still, this combo is prescribed too often.
Who’s at Highest Risk?
You don’t have to be elderly to be at risk. But if you fit any of these, you’re in the danger zone:
- Taking five or more medications daily
- Have kidney or liver disease (eGFR under 30 or elevated liver enzymes)
- Are over 65 - 45% of this group takes four or more drugs
- Use supplements or herbal products
- See multiple doctors without sharing medication lists
People with liver or kidney problems are 2.5 to 4 times more likely to have serious interactions. Why? Because their bodies can’t clear drugs the way a healthy one can. A dose that’s safe for someone else might be a poison for them.
What You Can Do: A Practical Action Plan
Managing interactions isn’t just your doctor’s job. You have power here. Here’s how to use it:
1. Keep a Real Medication List
Not a mental list. Not a scrap of paper. A real, updated list. Include:
- Every prescription (name, dose, why you take it)
- Every OTC pill - ibuprofen, antacids, sleep aids
- All supplements - vitamins, fish oil, St. John’s Wort, magnesium
- Recreational substances - alcohol, marijuana
Update it every time something changes. Bring it to every appointment. Pharmacists say this single step cuts interaction risks by 60%.
2. Ask Three Questions When Starting a New Drug
Don’t wait for your doctor to bring it up. Ask:
- “Could this interact with anything else I’m taking?”
- “Is there a safer alternative?”
- “What should I watch for in the first week?”
Doctors miss interactions 30-50% of the time. Especially when they’re rushed. Your questions make them slow down.
3. Know Your Enzymes
You don’t need to be a scientist. But you should know one thing: CYP3A4 is the most common enzyme involved in interactions. If your new drug is metabolized by it - and many are - then anything that blocks or speeds it up matters.
Blockers (inhibitors) = higher drug levels: grapefruit juice, clarithromycin, fluconazole, diltiazem
Speeders (inducers) = lower drug levels: St. John’s Wort, rifampin, carbamazepine, chronic alcohol use
If your doctor says, “This might affect your other meds,” ask: “Is it CYP3A4?” That tells you how serious it is.
4. Get a Medication Review
Most pharmacies offer free medication reviews. Use them. Especially after hospital discharge. A 2023 Mayo Clinic study showed pharmacist-led reviews cut readmissions by 22%. They don’t just check for interactions. They spot duplicates, wrong doses, and pills you’ve been taking for years with no reason.
5. Watch for Early Warning Signs
Don’t wait for a hospital visit. Watch for these in the first 7-10 days:
- Unusual bruising or bleeding
- Extreme drowsiness or confusion
- Unexplained muscle pain or weakness
- Swelling in ankles or face
- Heart palpitations or sudden dizziness
If you notice any of these, call your pharmacist or doctor. Don’t wait. Don’t Google it. Call.
Why Electronic Alerts Fail (And What to Do Instead)
Hospitals and clinics use software to warn doctors about interactions. But here’s the problem: physicians override 90-95% of alerts. Why? Too many false alarms. Too many pop-ups. Too many warnings for tiny risks.
Studies show only high-severity alerts - the ones that say “contraindicated” or “50% dose reduction required” - get real attention. So don’t rely on your EHR to catch everything.
Your best defense? A human. A pharmacist. A clear list. A conversation. Technology helps. But it doesn’t replace you.
What About Supplements and Natural Products?
“Natural” doesn’t mean safe. St. John’s Wort is the biggest offender. But others matter too:
- Grapefruit juice - Blocks CYP3A4. Affects over 85 drugs, including some statins, blood pressure meds, and immunosuppressants.
- Garlic and ginkgo - Thin blood. Dangerous with warfarin or aspirin.
- Calcium and iron supplements - Can block absorption of thyroid meds or antibiotics like ciprofloxacin. Take them 4 hours apart.
One survey found 68% of patients never mention supplements to their doctors. That’s not oversight. That’s a silent risk.
When in Doubt, Pause
There’s no shame in saying: “I’m not sure about this combo. Let me check.”
Pharmacists are trained for this. They use tools like the Liverpool HIV Interaction Scale and the ICH M12 guidelines - the same ones used by drugmakers and regulators. If your doctor is unsure, ask for a pharmacist consult. Most clinics offer it now. Use it.
And if you’re ever confused about instructions - like “take on an empty stomach” - ask. University of Michigan found 32% of patients misunderstand this. It doesn’t mean “don’t eat for two hours.” It means: take it one hour before eating, or two hours after.
Final Thought: You’re the Center of Your Care
Medications are powerful. But they’re not magic. They interact with your body, your other drugs, your diet, even your habits. Starting a new one isn’t just about taking a pill. It’s about understanding how it fits into the whole system.
The tools exist. The knowledge is out there. The experts are ready. But they can’t help if you don’t speak up.
Keep your list. Ask your questions. Trust your gut. If something feels off in the first week - it probably is. Don’t ignore it.
Can I still take grapefruit juice if I’m on a new medication?
No - not if you’re taking any of these: simvastatin, atorvastatin, felodipine, cyclosporine, or some anti-anxiety drugs. Grapefruit juice blocks the CYP3A4 enzyme, which can cause drug levels to spike dangerously. Even one glass can have effects for 24 hours. If you’re unsure, check with your pharmacist. Safer alternatives? Orange juice (not grapefruit) or water.
How long should I wait between taking supplements and my prescriptions?
For calcium, iron, or antacids: wait at least 4 hours before or after taking thyroid meds (like levothyroxine), antibiotics (like ciprofloxacin), or bisphosphonates (like alendronate). For most other supplements, a 2-hour gap is enough. But if you’re on warfarin, digoxin, or immunosuppressants - always check. Timing matters more than you think.
Do all pharmacies check for interactions?
No. Only about 35% of community pharmacies offer full medication reviews. Chain pharmacies often just check for obvious conflicts. If you’re on five or more drugs, ask specifically for a comprehensive review. It’s free, takes 15-20 minutes, and can catch hidden risks your doctor missed.
I’m on warfarin. Should I avoid vitamin K-rich foods?
No - but be consistent. Vitamin K (in leafy greens, broccoli, Brussels sprouts) counteracts warfarin. If you suddenly eat a lot of kale one week and none the next, your INR will swing wildly. The goal isn’t to avoid it - it’s to keep your intake steady. Talk to your provider about a daily amount that works for you.
Can I stop a medication if I think it’s interacting?
Never stop a prescription without talking to your doctor. Stopping suddenly can cause withdrawal, rebound effects, or worsen your condition. If you suspect an interaction, call your pharmacist or prescriber. They can help you adjust safely - sometimes by switching to a different drug, changing the dose, or spacing out timing.
Starting a new medication is a step toward better health. But without awareness, it can become a risk. The system isn’t perfect. Alerts fail. Doctors miss things. But you - with your list, your questions, and your voice - can be the missing piece that keeps you safe.
10 Comments
Brad Ralph
Grapefruit juice and statins? Yeah, I learned that the hard way. My dad ended up in the ER after a glass of OJ and a 40mg simvastatin. Turned out the juice wasn’t OJ-it was grapefruit. He didn’t even know the difference. 🍊💀
Stacie Willhite
This post saved me. I’ve been on 7 meds since my heart surgery and never thought to ask about interactions. I printed out your list and brought it to my pharmacist last week. She caught two duplicates I didn’t even know I was taking. Thank you for writing this.
Vamsi Krishna
LMAO so you’re telling me I can’t have my morning grapefruit while on my blood pressure med? Bro, I’ve been eating it for 15 years. You think I’m gonna stop because some guy in a lab coat said so? I’ve got more sense than your EHR. 🤷♂️
Sonja Stoces
Oh wow. So YOU’RE the one who thinks supplements are dangerous? I’ve been taking 14 different herbs and 5 vitamins since 2019. My bloodwork? Perfect. Your ‘science’ is just Big Pharma fearmongering. 🙄
Annie Joyce
I work as a pharmacy tech. I see this EVERY DAY. A man came in last Tuesday asking if he could take his St. John’s Wort with his SSRI. I said ‘no’ and he said ‘but it’s natural!’ I told him, ‘so is arsenic.’ He left mad. But he came back 3 days later with his wife. She made him listen. 🙏
Jason Pascoe
I’m from Australia and we have this thing called ‘Medication Management Reviews’ through Medicare. Free, 20-minute session with a pharmacist. They go through every pill, supplement, and ‘natural remedy’ you’ve ever taken. If you’re on 5+ meds, do it. It’s like a reset button for your health. I did it last year-found out I’d been taking two different versions of the same blood pressure pill. Oops.
christian jon
I can’t believe this post didn’t mention the REAL villain: THE DOCTOR. I’ve been on warfarin for 8 years. My last GP prescribed me amiodarone WITHOUT checking my med list. I had to go to the ER because my INR hit 9.8. The pharmacist had to call the doctor and scream at him. Why do we even have EHRs if they’re just for show? Someone needs to get fired. #HealthcareFail
Rob Turner
I’m from the UK and we don’t have grapefruit juice here much-but we do have something called ‘paracetamol’ (you guys call it Tylenol). Anyway, I had a mate who took 10 of them a day for his back pain. Said ‘it’s natural, man.’ He ended up with liver failure. The point? ‘Natural’ doesn’t mean ‘harmless.’ We’ve all got a bit of ‘I know what’s best’ in us. But this? This is why we need to pause. 🇬🇧❤️
Luke Trouten
The CYP3A4 enzyme is responsible for metabolizing over 50% of clinically used drugs. Its inhibition by grapefruit juice is well-documented in pharmacokinetic literature since the 1990s. The mechanism involves irreversible binding to intestinal CYP3A4, leading to reduced first-pass metabolism. This is not anecdotal-it’s foundational to clinical pharmacology. The fact that patients still don’t know this speaks to systemic failures in patient education.
Gabriella Adams
I’m a nurse practitioner. I read this whole thing. I cried. Not because it’s sad-but because it’s so true. I had a patient last month who took St. John’s Wort with her birth control. Got pregnant. She didn’t tell me because she thought it was ‘just a herb.’ We need to stop treating supplements like harmless candy. Thank you for writing this. I’m printing 20 copies for my clinic.

Write a comment