Lifestyle Changes to Reduce Medication Side Effects: Practical Guide

Medication Lifestyle Interaction Checker
How Your Habits Affect Your Medications
The article explains how your daily habits can worsen or improve medication side effects. This tool helps you identify potential interactions between your medications and lifestyle choices.
Many people take medications to manage chronic conditions-high blood pressure, diabetes, depression, cholesterol-but they often blame the drugs when things go wrong. Fatigue, nausea, weight gain, muscle pain, dizziness-these aren’t always the medication’s fault. Sometimes, they’re the result of how you live. The truth is, your daily habits can make side effects worse… or help them disappear.
How Your Daily Habits Interact With Your Medications
Your body doesn’t treat medication like a magic bullet. It processes drugs through your liver, kidneys, and gut-all of which are influenced by what you eat, how you sleep, how much you move, and how you handle stress. A 2021 study in JAMA Internal Medicine found that side effects from medications contribute to nearly 7% of hospital admissions. That’s not because the drugs are dangerous. It’s because lifestyle factors are out of sync with them. For example, if you’re on a statin for high cholesterol and you eat grapefruit every morning, you’re increasing the drug’s concentration in your blood by up to 50%. That raises your risk of muscle pain without giving you extra benefit. Or if you’re taking metformin for diabetes and you skip meals or binge on carbs, you’re more likely to get stomach cramps and diarrhea. These aren’t random side effects-they’re predictable reactions to your habits. The good news? You can often fix this without changing your meds. The American College of Lifestyle Medicine and the American Medical Association both agree: lifestyle changes aren’t alternatives to medication-they’re force multipliers. When done right, they let you take lower doses, feel better, and avoid hospital visits.Move More to Cut Fatigue and Muscle Pain
If you’re on beta-blockers for high blood pressure or heart disease, you might feel tired all the time. It’s a common complaint. But research from the American Heart Association shows that starting a gentle exercise routine can reverse this. Begin with just 10 minutes of walking twice a day. After eight weeks, most people report a 41% boost in energy. Same goes for statin-related muscle pain. About 1 in 4 people on statins experience this. A 2021 study in the Journal of the American College of Cardiology found that adding 200mg of coenzyme Q10 daily and doing two 10-repetition strength sessions per week (using light weights) cut muscle pain from 29% to just 11%. That’s not luck-it’s biology. Statins lower your body’s natural CoQ10, which your muscles need to produce energy. Replacing it helps. You don’t need to run marathons. Consistency matters more than intensity. Aim for 150 minutes a week of brisk walking, cycling, or swimming. That’s 30 minutes, five days a week. It’s enough to improve how your liver processes drugs, reduce inflammation, and help your muscles recover.Eat Smart to Avoid Nausea, Weight Gain, and Drug Interactions
What you eat doesn’t just affect your weight-it affects how your body handles medicine. Take GLP-1 agonists like semaglutide (Ozempic, Wegovy). These drugs help with weight loss and blood sugar control, but up to 73% of people get nausea when they start. A 2023 study found that changing how you eat cuts that number in half. Slow down. Eat smaller meals (under 500 calories). Avoid spicy or acidic foods. Don’t eat within three hours of bedtime. Drink at least 2.2 liters of water daily if you’re a woman, 3 liters if you’re a man. Do all that, and nausea drops to 29%. If you’re on warfarin (a blood thinner), watch your leafy greens. Kale, spinach, broccoli-these are high in vitamin K, which directly counteracts warfarin. Eating 150mcg or more of vitamin K daily can reduce the drug’s effect by 30-50%. That’s dangerous. You don’t need to avoid these foods entirely. Just keep your intake consistent. If you eat spinach every day, keep doing it. If you rarely eat it, don’t suddenly start. Grapefruit juice is another big one. It blocks an enzyme (CYP3A4) that breaks down many drugs-statins, blood pressure meds, some antidepressants. One glass a day can spike drug levels enough to cause side effects. Skip it. Or switch to orange juice. For antidepressant-related weight gain, the fix is protein and movement. A 2022 study found that people who ate 1.6 grams of protein per kilogram of body weight daily (about 30g per meal) and exercised 150 minutes a week gained only 1.5 pounds in the first year. Those who didn’t gained over 7 pounds. Protein keeps you full, stabilizes blood sugar, and helps preserve muscle while losing fat.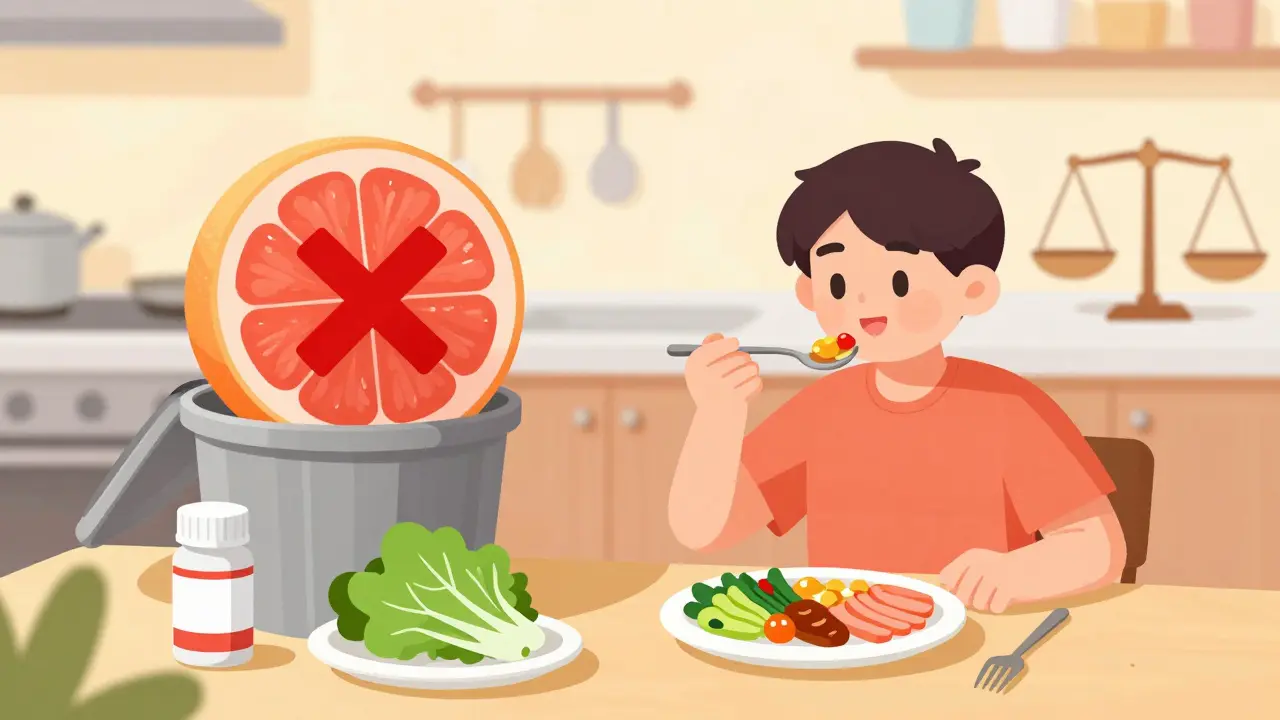
Sleep Better to Improve Drug Metabolism
You’ve probably heard that sleep is important. But did you know it directly affects how your body breaks down medication? The liver uses enzymes to process most drugs. These enzymes work best when you’re sleeping. A 2022 study from the National Sleep Foundation showed that people who got 7-9 hours of quality sleep each night metabolized drugs like statins and antidepressants 22% faster. That means less buildup in your system, fewer side effects, and better results. Poor sleep also raises cortisol-the stress hormone-which can worsen insulin resistance, raise blood pressure, and make antidepressants less effective. If you’re on medication for anxiety or depression, sleep isn’t optional. It’s part of the treatment. Start with a simple routine: go to bed and wake up at the same time every day-even on weekends. Keep your room cool and dark. Avoid screens an hour before bed. If you’re still struggling, talk to your doctor about sleep hygiene. It’s not just about feeling rested-it’s about making your meds work better.Manage Stress to Boost Mental Health Meds
Stress doesn’t just make you feel anxious. It changes your brain chemistry in ways that interfere with antidepressants and anti-anxiety medications. A 2021 study in JAMA Psychiatry found that people who practiced 30 minutes of mindfulness meditation daily lowered their cortisol levels by 27%. That led to a 31% improvement in antidepressant effectiveness and fewer side effects like weight gain, drowsiness, and emotional numbness. You don’t need to sit cross-legged for an hour. Try this: take five deep breaths when you wake up. Walk without your phone for 10 minutes. Listen to calming music. Journal for five minutes before bed. These aren’t fluffy wellness tips-they’re biological interventions. Stress also affects blood pressure meds. If you’re chronically tense, your body releases adrenaline, which raises your blood pressure. That makes your pills less effective. Managing stress isn’t a luxury-it’s a medical necessity.Timing Matters More Than You Think
When you take your meds matters as much as what you take. Statins work best at night because your liver makes most cholesterol while you sleep. Taking them in the morning cuts their effectiveness. Blood pressure pills? Some work better in the morning, others at night. A 2022 study found that taking at least one blood pressure med at bedtime reduced heart attacks and strokes by 34% compared to taking them all in the morning. Metformin should be taken with meals to reduce stomach upset. GLP-1 agonists are often taken once a week, but if you’re starting out, your doctor might advise taking them on a day when you have fewer social obligations-because nausea can hit hard. If you’re on multiple meds, use a pill organizer. Set phone alarms. Don’t assume your doctor will remind you. Most don’t have time. You need to be your own advocate.What to Do Next: A Simple 4-Step Plan
You don’t need to overhaul your life overnight. Start small. Pick one area and stick with it for 30 days.- Track your meds and symptoms. For one week, write down what you take, when, and how you feel afterward. Are you tired after lunch? Nauseous after dinner? Jot it down.
- Choose one lifestyle change. Pick the one that’s easiest: walk 20 minutes a day. Drink more water. Eat dinner earlier. Cut grapefruit juice.
- Stick with it for 30 days. Don’t change anything else. Let your body adjust.
- Check in with your doctor. Bring your notes. Ask: “Could this lifestyle change help me lower my dose?”
What Not to Do
Don’t stop your meds because you think lifestyle changes will fix everything. That’s dangerous. Blood pressure can spike. Blood sugar can soar. Depression can return with force. Don’t assume your doctor knows about your habits. Most don’t ask. Only 38% of primary care visits include any lifestyle assessment, even though 76% of patients take two or more medications with known lifestyle interactions. Don’t trust internet advice. “Natural remedies” that claim to replace your meds can be harmful. Coconut oil won’t lower your cholesterol like a statin. Turmeric won’t replace your blood thinner. Stick to science-backed changes.Final Thought: You’re Not Broken
If you’re struggling with side effects, it’s not because you’re weak, lazy, or failing. It’s because your body is responding to the signals you’re giving it. Medications are powerful-but they’re not magic. They work best when your lifestyle supports them. The goal isn’t to become a perfect health guru. It’s to make small, smart choices that help your body do its job. Move more. Eat mindfully. Sleep deeply. Manage stress. These aren’t add-ons. They’re part of your treatment plan. And when you do, you might find you don’t need as much medication after all.Can lifestyle changes replace my medication?
No. Lifestyle changes should support your medication, not replace it. Stopping meds without medical supervision can lead to serious health risks like rebound hypertension, uncontrolled diabetes, or worsening depression. Always talk to your doctor before making any changes to your treatment plan.
How long does it take for lifestyle changes to reduce side effects?
Most people notice improvements in 4 to 8 weeks. For example, exercise can reduce statin muscle pain in 8 weeks. Better sleep improves drug metabolism within 30 days. Nausea from GLP-1 agonists often drops within 2-4 weeks of eating slower and smaller meals. Consistency matters more than speed.
What foods should I avoid with my meds?
Avoid grapefruit juice with statins, blood pressure meds, and some antidepressants-it can spike drug levels dangerously. Limit vitamin K-rich foods (kale, spinach, broccoli) if you’re on warfarin-keep your intake consistent. High-sodium foods can reduce the effect of blood pressure pills. Always ask your pharmacist or doctor about food interactions for your specific meds.
Does alcohol affect medication side effects?
Yes. Alcohol can increase drowsiness with sedatives, raise blood pressure with some heart meds, and overload your liver when combined with painkillers like acetaminophen. It can also worsen depression and interfere with sleep. If you drink, do so in moderation and always check with your doctor about your specific medications.
Should I take supplements to reduce side effects?
Some, like coenzyme Q10 for statin muscle pain, have strong evidence. Others, like magnesium for blood pressure, may help but aren’t proven to replace meds. Never start a supplement without talking to your doctor-they can interact with your prescriptions. CoQ10 is generally safe, but others like St. John’s Wort can dangerously reduce the effect of antidepressants and birth control pills.
My doctor never talks about lifestyle changes. What should I do?
Bring it up. Say: “I’ve been reading about how diet, sleep, and exercise affect how my meds work. Could we talk about whether any changes might help me reduce side effects or lower my dose?” Many doctors want to help but don’t have time. Your initiative can spark the conversation. You can also ask for a referral to a certified health coach or dietitian.
14 Comments
Gerald Tardif
Been on statins for 5 years. Started walking 20 mins after dinner-no more muscle cramps. Didn’t even need CoQ10. Funny how the fix was just moving when I felt too tired to move.
Turns out, my body wasn’t broken. I was just sitting on it.
Monika Naumann
It is truly lamentable that modern medicine has devolved into a mere adjunct to dietary compliance. In my homeland, we honor the wisdom of ancestral healing-herbs, fasting, and spiritual discipline. To reduce medication dosage based on lifestyle is not innovation-it is regression to pre-scientific ignorance.
Will Neitzer
This is one of the most clinically nuanced pieces I’ve read in years. The integration of pharmacokinetics with behavioral science is not just sound-it’s essential. The JAMA and AHA citations are impeccable, and the 4-step plan is textbook patient-centered care. Kudos to the author for framing lifestyle as a pharmacological multiplier, not a substitute. This should be required reading for all primary care residents.
Olivia Goolsby
Wait-so you’re telling me the pharmaceutical industry doesn’t want us to fix our lifestyles because then we’d stop buying their pills? And the FDA? They’re in bed with Big Pharma. And the doctors? They’re paid by drug reps to keep you dependent. Grapefruit juice? That’s just the tip of the iceberg. Did you know they add fluoride to water to mess with your liver enzymes so you need MORE meds? And CoQ10? They banned it in 1998 in 14 countries because it works too well. I’ve been tracking my meds since 2017-every single side effect? Manufactured. They profit from your suffering. Wake up.
Liz Tanner
I was on antidepressants for 8 years and gained 30 pounds. Started eating protein at every meal and walking with my dog every morning. Lost 22 pounds in 6 months. My doctor was shocked. I didn’t stop my meds-I just gave my body what it needed to use them better. You’re not weak for needing help. You’re human. And humans need food, movement, rest. It’s not complicated.
Satyakki Bhattacharjee
Life is simple. Eat less. Sleep more. Walk. Stop being lazy. Medicine is for weak minds. Real men and women fix themselves with discipline. Why do you think the old people lived to 90? They didn’t have pills. They had will.
Kishor Raibole
While the empirical data presented is commendable, one must not overlook the systemic erosion of personal agency in contemporary healthcare. The notion that one’s metabolic fate is subject to the whims of circadian rhythm and dietary compliance-rather than the divine order of bodily equilibrium-reflects a troubling anthropocentric reductionism. One cannot reduce the soul’s harmony to the enzymatic kinetics of the hepatic parenchyma.
John Barron
OMG I’ve been doing ALL of this and my doctor still won’t lower my dose 😭 I took CoQ10, stopped grapefruit, walked 5 days a week, slept 8 hours, meditated, used a pill organizer, and STILL they say ‘it’s fine’… I think they just don’t care. Like, I’m literally doing everything right and they treat me like I’m asking for a candy bar. #MedicationStruggles #PharmaIsTheProblem 💔💊
Liz MENDOZA
Thank you for writing this. I’ve been too scared to talk to my doctor about my habits because I felt judged. But this made me feel seen. I’ve been eating dinner at 10pm because I work late, and I didn’t realize that was wrecking my antidepressants. I’m starting tonight. No pressure. Just one small change. And I’m proud of myself already.
Anna Weitz
They say lifestyle fixes side effects but they never mention that your body adapts to the meds first. You think walking helps? It just means your liver gets used to the drug and you need more. This whole thing is a cycle. You fix one thing and the system compensates. The only real solution is detoxing your environment. No plastics. No processed food. No screens. No meds. That’s the truth they don’t want you to know
Jane Lucas
i just started taking metformin and was terrified of the stomach stuff… but i’ve been eating smaller meals and drinking water like a normal human and it’s been fine. no drama. no magic. just… eating like my body asked me to. who knew?
Elizabeth Alvarez
They’re hiding the truth. The real reason side effects happen is because the meds are laced with microchips to track your behavior. That’s why they say ‘sleep better’-because the chip needs to sync with your circadian rhythm to send data to the cloud. CoQ10? It blocks the signal. Grapefruit? It fries the antenna. The study they cite? Funded by the same people who own the drug companies and the sleep trackers. You think you’re fixing your life-you’re just feeding the algorithm.
Miriam Piro
Everything they say about lifestyle is true… but only because the government and Big Pharma already know that if people just ate better and slept enough, they’d stop buying drugs. So they made it seem like a ‘choice’-a personal responsibility-so you feel guilty when you fail. But the truth? The system is designed to keep you sick. The ‘4-step plan’? It’s a trap. It makes you think you’re in control… when really, you’re just a data point in their profit model. Wake up. They don’t want you healthy. They want you compliant.
Gerald Tardif
Just read the guy who said ‘real men fix themselves with discipline.’ I’ve been on beta-blockers since I was 35. I’ve got two kids, a full-time job, and a bad back. I didn’t have time for ‘discipline.’ I had time for 10-minute walks. That’s all it took. You don’t need to be a hero. You just need to show up. Even a little.

Write a comment