Osteodystrophy and Fracture Risk: What You Need to Know
Understanding Osteodystrophy and Its Impact on Bone Health
Osteodystrophy is a medical condition that affects our bones, making them weak and prone to fractures. It is often seen in people suffering from chronic kidney disease, as their body is unable to properly regulate calcium and phosphorus levels. In this section, we will delve into the basics of osteodystrophy, its causes, and how it can lead to an increased risk of fractures.
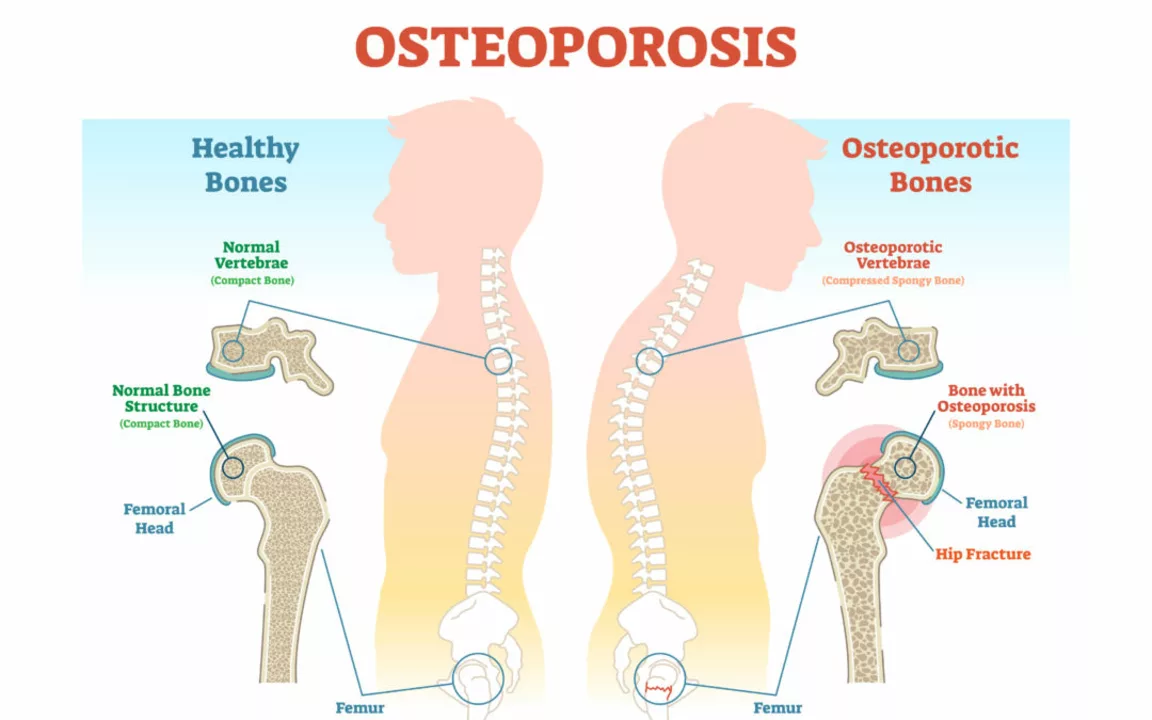
Our bones are constantly in a state of renewal, with old bone being broken down and new bone being formed. This process is called bone remodeling. However, in people with osteodystrophy, this delicate balance is disrupted, resulting in a higher rate of bone breakdown than bone formation. As a result, the bones become weak, thin, and more susceptible to fractures.
There are many factors that can contribute to the development of osteodystrophy, including hormonal imbalances, vitamin D deficiency, and certain medications. Understanding the underlying causes of this condition is crucial in managing and preventing complications, such as fractures.
Recognizing the Symptoms of Osteodystrophy
One of the most challenging aspects of osteodystrophy is that it often does not present any noticeable symptoms in its early stages. This makes it difficult to diagnose and treat before significant damage has occurred. However, as the condition progresses, certain signs and symptoms may become more evident.
Common symptoms of osteodystrophy include bone pain, joint pain, muscle weakness, and deformities in the bones. In more advanced cases, individuals may also experience fractures with little or no trauma, which can be a clear indication of weakened bone structure.
If you are experiencing any of these symptoms, it is important to consult with your healthcare provider for proper assessment and diagnosis. Early detection and treatment can help to minimize the risk of fractures and other complications associated with osteodystrophy.
Assessing Your Fracture Risk
Given the increased risk of fractures in individuals with osteodystrophy, it is crucial to assess your personal fracture risk. This can be done through a combination of medical history, physical examination, and various diagnostic tests.
Your healthcare provider may perform a bone density test, which measures the amount of minerals in your bones and can help to determine the likelihood of fractures. Additionally, blood tests may be performed to check for imbalances in calcium, phosphorus, and vitamin D levels, which can be contributing factors to osteodystrophy.
By understanding your individual fracture risk, you and your healthcare provider can work together to develop an appropriate treatment plan to help prevent fractures and maintain your overall bone health.
Managing Osteodystrophy through Diet and Lifestyle
One of the most effective ways to manage osteodystrophy and reduce the risk of fractures is through proper diet and lifestyle changes. Ensuring that you are consuming an adequate amount of calcium and vitamin D is crucial for maintaining strong and healthy bones.
Some good sources of calcium include dairy products, leafy green vegetables, and fortified foods. Vitamin D can be obtained through exposure to sunlight, as well as through certain foods, such as fatty fish and fortified milk. In some cases, your healthcare provider may recommend supplements to help meet your nutritional needs.
Additionally, engaging in regular weight-bearing exercise, such as walking, jogging, or resistance training, can help to strengthen your bones and reduce the risk of fractures. However, it is important to consult with your healthcare provider before beginning any new exercise routine to ensure that it is safe and appropriate for your individual needs.
Medical Treatment Options for Osteodystrophy
Depending on the severity of your osteodystrophy and your individual risk factors, your healthcare provider may recommend certain medical treatments to help manage the condition and reduce the risk of fractures. These may include medications, such as bisphosphonates, which help to slow down bone breakdown and promote bone formation.
In some cases, hormone replacement therapy may be recommended, particularly for individuals with hormone imbalances contributing to their osteodystrophy. Additionally, individuals with chronic kidney disease may require specific treatments to manage their condition and prevent further complications related to osteodystrophy.
It is important to work closely with your healthcare provider to determine the most appropriate treatment options for your specific needs and to closely monitor your progress to ensure optimal bone health.
Living with Osteodystrophy: Tips for Maintaining Bone Health
Living with osteodystrophy can be challenging, but with the right approach, you can maintain your bone health and reduce the risk of fractures. Here are some tips to help you manage your condition and maintain a high quality of life:
1. Stay informed: Educate yourself about osteodystrophy and stay up-to-date on the latest research and treatment options.
2. Follow your treatment plan: Work closely with your healthcare provider to develop a comprehensive treatment plan and be diligent in following it.
3. Prioritize nutrition: Ensure that you are consuming a balanced diet rich in calcium, vitamin D, and other essential nutrients for bone health.
4. Stay active: Engage in regular weight-bearing exercise, as recommended by your healthcare provider, to help strengthen your bones and reduce the risk of fractures.
5. Monitor your progress: Regularly assess your fracture risk and work with your healthcare provider to make any necessary adjustments to your treatment plan.
6. Be proactive: Take steps to prevent falls and accidents that may result in fractures, such as removing trip hazards in your home and ensuring that you have proper footwear.
By following these tips and working closely with your healthcare provider, you can effectively manage your osteodystrophy, maintain your bone health, and reduce the risk of fractures. Remember, early detection and intervention are key to preventing complications and ensuring the best possible outcome.
18 Comments
Josh Grabenstein
Bones are just scaffolding the powers don’t want you to think about 🤔
Marilyn Decalo
Wow, another “miracle” article about bones! As if the medical industry hasn’t been pulling the wool over our eyes for years. The whole “calcium and vitamin D” spiel is just a blockbuster marketing ploy. I mean, why would anyone actually trust that bland advice when the truth is out there? Cue the drama of a broken hip that could've been avoided-if only we’d listen to the whispers.
Mary Louise Leonardo
They tell us to drink milk, but did you know the big dairy lobby feeds us secret chemicals? My grandma said the “white powder” isn’t just calcium – it’s control. Bones getting weak is part of the plan to keep us dependent on pharma. Stay alert, stay strong.
Alex Bennett
Ah, the age‑old dance between decay and renewal; one might say our skeletons are the ultimate philosophers, questioning their own existence. It’s mildly amusing that we need to tell them to lift weights, as if they’d know the difference. Still, a balanced diet and some resistance training won’t hurt-unless you enjoy the irony of a broken arm.
Mica Massenburg
Did anyone notice how the labs that run bone density tests are owned by the same corporations that sell supplements? I’m not saying they’re lying, but why else would the numbers always hover just above the danger line? Just a thought.
Sarah Brown
Managing osteodystrophy takes more than reading a glossy article-you need a solid plan.
First, get your labs checked every three months; calcium, phosphorus, and vitamin D levels fluctuate wildly in kidney disease.
If any value is out of range, demand a dose adjustment from your doctor-don’t accept “close enough.”
Second, schedule a DXA scan and keep a copy of the report; track the T‑score over time.
Third, adopt a diet rich in calcium but low in phosphorus, focusing on leafy greens, fortified plant milks, and low‑phosphate proteins.
Fourth, incorporate weight‑bearing exercises at least three times a week-think brisk walks, stair climbs, or resistance bands.
Fifth, consider a bisphosphonate after reviewing the risks; discuss it thoroughly with your nephrologist.
Sixth, if you’re on steroids or have hormonal imbalances, request a hormone panel-sometimes adrenal issues are the hidden culprits.
Seventh, stay vigilant for any sudden pain or bruising; a fracture can happen with minimal trauma.
Eighth, protect your home environment-remove loose rugs, install grab bars, and wear supportive footwear.
Ninth, keep a medication list that includes over‑the‑counter supplements; interactions can sabotage your bone health.
Tenth, lean on a support group-sharing experiences can reveal practical tips you won’t find in journals.
Eleventh, track your progress in a notebook or app; seeing incremental gains keeps you motivated.
Twelfth, never let anyone tell you that “it’s just aging”; osteoporosis and osteodystrophy are medical conditions you can combat.
Finally, celebrate small victories-a pain‑free day, a new personal record on the treadmill-and keep pushing forward.
Max Canning
Yo, this stuff sounds intense but trust me, you can crush it! Grab some sunshine, munch on broccoli, and hit the park-your bones will thank you. Let’s get moving, fam!
Nick Rogers
It is advisable, therefore, to maintain adequate calcium intake, to ensure regular physical activity, and to monitor renal function, as these measures collectively reduce fracture risk.
Tesia Hardy
i think sarah’s list is gold, but also try adding a little yoga for balance-i’ve seen it help friends stay steadier, so yeah keep it up and stay positive!
Matt Quirie
While the recommendations presented are comprehensive, it would be prudent, for the sake of thoroughness, to also consider the potential benefits of emerging therapies, such as sclerostin inhibitors, in future management plans.
Pat Davis
Indeed, the pragmatic approach of combining sunlight exposure with weight‑bearing activity aligns well with contemporary guidelines, and I encourage patients to adopt these practices without delay.
Mary Wrobel
Hey folks, think of your bones as a vibrant garden; sprinkle in some dairy blossoms, let the sun kiss you, and watch that sturdy oak of health grow tall and proud.
Lauren Ulm
Ever wonder why the “big pharma” keeps pushing calcium pills? 🤔 It’s almost as if they’re feeding us sugar‑coated control while our skeletons silently rebel. 🌟 Stay curious, stay strong.
Michael Mendelson
One must-admittedly-acquiesce to the notion that modern medicine, albeit riddled with bourgeois trivialities, offers a scintillating array of therapeutics; yet, it’s frequently obscured by the cacophony of lowbrow marketing.
Ibrahim Lawan
It is essential, from a physiological standpoint, to balance mineral homeostasis while implementing progressive resistance training, thereby optimizing bone remodeling cycles in patients with renal osteodystrophy.
Just Sarah
May I inquire as to the specific pharmacokinetic parameters of bisphosphonate administration in the context of chronic kidney disease; furthermore, could the author elucidate the comparative efficacy of denosumab versus traditional agents, taking into account longitudinal bone mineral density outcomes?
Anthony Cannon
Consider the evidence: calcium, vitamin D, exercise and monitoring reduce fracture risk effectively.
Kristie Barnes
just a gentle reminder to listen to your body, take things one step at a time, and know that you’re not alone in this journey.






Write a comment