Antispasmodics and Anticholinergic Drug Interactions: What You Need to Know

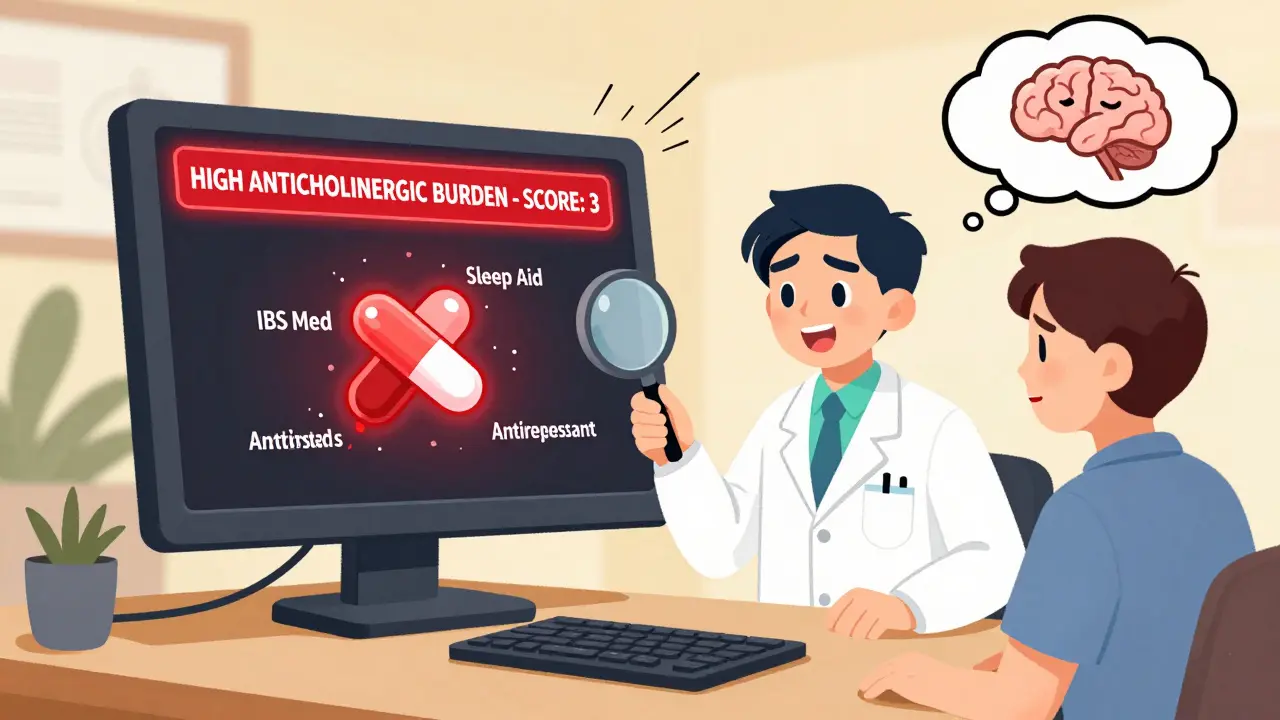
Anticholinergic Burden Calculator
How to Use This Tool
Enter medications you're currently taking. This tool calculates your total anticholinergic burden score based on standard medical guidelines. Scores of 2 or higher indicate high risk.
Note: This tool is for educational purposes only. Always consult your doctor or pharmacist about your medications.
Your Current Medications
Results
Many people take antispasmodics to ease stomach cramps, bladder spasms, or irritable bowel symptoms. But what they don’t always realize is that these medications can turn dangerous when mixed with other common drugs. The problem isn’t just one or two bad combinations-it’s a quiet, widespread risk built into how these drugs work. Antispasmodics like dicyclomine and hyoscine block acetylcholine, a chemical your body uses to control muscle contractions. That’s why they help with spasms. But that same mechanism means they can clash badly with dozens of other medications, especially in older adults or those taking multiple prescriptions.
How Anticholinergic Antispasmodics Work-and Why They Clash
These drugs don’t just relax muscles. They interfere with the parasympathetic nervous system, which controls involuntary functions like digestion, urination, and heart rate. By blocking acetylcholine at muscarinic receptors, they reduce spasms in the gut or bladder. But that same blockade affects saliva, vision, bladder emptying, and even brain function. Side effects like dry mouth, blurry vision, constipation, and urinary retention aren’t just annoyances-they’re warning signs the drug is working too hard.The real danger comes when you add another anticholinergic drug. Think of it like turning up the volume on a speaker that’s already at max. If you take dicyclomine for IBS and also take diphenhydramine (Benadryl) for allergies, you’re doubling the anticholinergic effect. That’s not just a theory-it’s what patients report. One user on Drugs.com described severe constipation after starting amitriptyline for nerve pain while already on dicyclomine. Another said they felt confused and had blurred vision after combining oxybutynin (for overactive bladder) with Benadryl. These aren’t rare cases. Pharmacists on Reddit say they’ve intervened in multiple cases this year alone where different doctors prescribed overlapping anticholinergic drugs without realizing the risk.
Common Medications That Make Antispasmodics Riskier
You don’t need to be on a long list of prescriptions to be in danger. Many everyday drugs have hidden anticholinergic properties. Here are the most common culprits:- Antidepressants: Amitriptyline, nortriptyline, paroxetine, and clomipramine all have strong anticholinergic effects.
- Antihistamines: Diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine are in many cold, allergy, and sleep aids.
- Antipsychotics: Quetiapine, clozapine, and olanzapine are used for schizophrenia and sometimes insomnia, but they carry high anticholinergic burden.
- Bladder medications: Oxybutynin, tolterodine, and solifenacin are prescribed for overactive bladder-same class as some antispasmodics.
- Sleep aids: Doxylamine, found in Unisom and many generic nighttime formulas, is a potent anticholinergic.
- Parkinson’s drugs: Trihexyphenidyl and benztropine are anticholinergics themselves.
It’s not just about taking two anticholinergics at once. Even one antispasmodic plus one of these can push you over the edge. A 2023 study in JAMA Internal Medicine found that when doctors used a digital tool to flag these combinations, inappropriate prescribing dropped by 43% across 12 hospitals. That tells you how often this is slipping through the cracks.
Who’s Most at Risk-and Why
Older adults are the most vulnerable group. Their bodies process drugs slower, their brains are more sensitive to acetylcholine disruption, and they’re more likely to be on multiple medications. The American Geriatrics Society Beers Criteria® lists several antispasmodics as potentially inappropriate for people over 65. Why? Because the risk of delirium, falls, confusion, and urinary retention skyrockets. One study showed that people over 65 taking three or more anticholinergic drugs had a 60% higher risk of dementia over 10 years.But it’s not just age. People with glaucoma, prostate problems, or constipation are also at higher risk. Anticholinergics can worsen narrow-angle glaucoma by increasing eye pressure. They can cause urinary retention in men with enlarged prostates. And if you already struggle with constipation, adding dicyclomine or hyoscine can turn it into a medical emergency.
What’s Changed in the Last Five Years
The medical community has woken up to this issue. In 2021, the American Gastroenterological Association said 68% of gastroenterologists now avoid anticholinergic antispasmodics as first-line treatment for IBS. Why? Because safer alternatives exist. Drugs like peppermint oil capsules, rifaximin, and even certain probiotics have proven effective without the interaction risks.Prescription trends reflect this shift. From 2018 to 2022, anticholinergic antispasmodic prescriptions dropped 22% in the U.S., while non-anticholinergic options rose 37%. The European Medicines Agency now requires explicit warnings on packaging about combining these drugs with CNS depressants like alcohol, benzodiazepines, or opioids. The FDA has boxed warnings for certain anticholinergics in patients with myasthenia gravis or obstructive uropathy.
Technology is catching up too. The University of Washington’s Anticholinergic Burden Calculator 2.0, released in 2022, now integrates with major electronic health records. It scores over 117 medications on a scale from low to high anticholinergic activity. If your total score hits 2 or higher, most systems now flag it as high-risk. That means your doctor’s computer might warn them before they even write the prescription.
What You Should Do Right Now
If you’re taking an antispasmodic, here’s what to check:- Review every medication you take. Include over-the-counter pills, supplements, and sleep aids. Look for ingredients like diphenhydramine, doxylamine, oxybutynin, or any drug ending in “-triptan” or “-dine.”
- Ask your pharmacist. Pharmacists have access to interaction checkers. Bring your full list-every pill, patch, or drop you use.
- Know your symptoms. Dry mouth? Constipation? Blurry vision? Trouble urinating? Confusion? These aren’t just side effects-they’re red flags.
- Ask about alternatives. Is there a non-anticholinergic option? Peppermint oil, fiber supplements, or even low-dose SSRIs like escitalopram (which has minimal anticholinergic effect) might work just as well.
Don’t stop your medication on your own. But do bring this conversation to your doctor. Many people assume their prescriptions are safe because they came from different specialists. That’s exactly how these dangerous combinations happen.
The Future: Safer Options Are Coming
Researchers are working on new antispasmodics that target only the gut or bladder without crossing into the brain. Two peripherally-acting agents are in Phase III trials as of late 2023. These could offer relief without the confusion, memory issues, or delirium risk. But until they’re available, the safest choice is often to avoid anticholinergics altogether-if possible.Antispasmodics still have a place. For some people, they’re the only thing that helps. But they’re no longer the go-to solution. The tide has turned. The data is clear. The warnings are everywhere. The question isn’t whether these drugs work-it’s whether the risk is worth it.
Can I take dicyclomine with Benadryl?
No. Both dicyclomine and Benadryl (diphenhydramine) are anticholinergic drugs. Taking them together can cause severe dry mouth, constipation, urinary retention, blurred vision, confusion, and even delirium, especially in older adults. This combination is considered high-risk and should be avoided.
Are antispasmodics safe for seniors?
Most anticholinergic antispasmodics like dicyclomine and hyoscine are listed in the American Geriatrics Society Beers Criteria® as potentially inappropriate for older adults. They increase the risk of falls, confusion, memory problems, and urinary retention. Safer alternatives exist, and many doctors now avoid prescribing them to patients over 65 unless absolutely necessary.
What are the signs of anticholinergic toxicity?
Signs include extreme dry mouth, difficulty swallowing, blurred vision, constipation, inability to urinate, rapid heartbeat, confusion, hallucinations, agitation, and memory loss. In severe cases, it can lead to seizures, coma, or death. If you experience any of these while taking an antispasmodic with another medication, seek medical help immediately.
Can I take hyoscine with antidepressants?
It depends on the antidepressant. Tricyclics like amitriptyline and nortriptyline have strong anticholinergic effects and should not be combined with hyoscine. SSRIs like sertraline or escitalopram have minimal anticholinergic activity and are generally safer, but you should still check with your doctor. Never combine without review.
Is there a test to measure anticholinergic burden?
Yes. The Anticholinergic Cognitive Burden Scale and the Anticholinergic Burden Calculator 2.0 are tools used by clinicians to score medications based on their anticholinergic strength. A score of 2 or higher is considered high risk. Many electronic health systems now automatically flag combinations that exceed this threshold.
What are safer alternatives to anticholinergic antispasmodics?
For irritable bowel syndrome, peppermint oil capsules, fiber supplements (like psyllium), and low-dose SSRIs have shown effectiveness without anticholinergic side effects. For bladder spasms, mirabegron is a non-anticholinergic option. For general cramping, heat therapy, dietary changes, and probiotics can help. Always discuss alternatives with your doctor before switching.
15 Comments
Lisa Cozad
My grandma was on dicyclomine and Benadryl for years-never realized how dangerous it was until she started hallucinating at 3 a.m. We switched her to peppermint oil and her brain cleared up in a week. So glad this post exists.
Saumya Roy Chaudhuri
Let me tell you something-this is why Indian doctors are better. We don't just throw pills at people. In my village, we use ginger tea, fennel seeds, and warm compresses. No chemicals. No confusion. No delirium. Western medicine is a factory line of side effects.
Ian Cheung
Man I used to take Benadryl like candy when I was 22-sleep, allergies, anxiety, you name it. Then I turned 35 and suddenly my brain felt like it was wrapped in cotton. Turns out I was on dicyclomine for IBS and didn't even know it was a double whammy. Now I just drink chamomile tea and chill. Best decision ever. Thanks for the wake-up call.
anthony martinez
Of course the FDA didn’t do anything until Big Pharma started losing money on anticholinergics. Now suddenly it’s a "public health crisis"-convenient.
Mario Bros
You got this. Seriously. Talking to your pharmacist is one of the smartest things you can do. I did it last year and they caught a triple anticholinergic combo I didn’t even know I was on. Saved me from a hospital trip. 🙌
Jake Nunez
In my family, we’ve been avoiding these drugs since my uncle got stuck in urinary retention for three days. Now we all ask: "Is this really necessary?" And if the answer isn’t clear, we wait. Patience beats poison any day.
Christine Milne
While I appreciate the anecdotal nature of this post, I must emphasize that the methodology behind the JAMA study cited is statistically flawed due to selection bias in the electronic health record data pool. Furthermore, the American Geriatrics Society Beers Criteria is not evidence-based-it is consensus-driven and therefore inherently subjective. One cannot extrapolate population trends to individual clinical outcomes without proper multivariate regression analysis.
Bradford Beardall
Has anyone tried the Anticholinergic Burden Calculator? I plugged in my meds and it flagged me at 3.5. My doctor was shocked-I thought I was just getting older. Now I’m on mirabegron and it’s been a game-changer. Also, why isn’t this tool mandatory in every EHR? It’s like we’re flying blind.
McCarthy Halverson
Check your OTC meds. That’s the big one. Benadryl in every sleep aid. Doxylamine in Unisom. People don’t even realize they’re taking anticholinergics daily. Just stop. Try melatonin instead.
Michael Marchio
Let’s be real here-this isn’t about drug interactions. This is about the medical-industrial complex pushing pills because they’re profitable. Antispasmodics have been around for decades. Why now? Because someone found a way to monetize "anticholinergic burden" as a new diagnostic category. The real problem? Doctors don’t listen. They don’t ask. They prescribe. And patients? They’re just trying to feel better. But now we’re supposed to memorize every drug ending in -dine and -triptan? That’s not healthcare. That’s a quiz show.
Jake Kelly
I’ve been on oxybutynin for years. After reading this, I talked to my urologist and switched to mirabegron. No dry mouth. No brain fog. Just peace. It’s not magic-it’s just smarter medicine.
Ashlee Montgomery
It’s funny how we treat the body like a machine that needs fixing instead of a system that needs balance. We block acetylcholine to stop cramps but forget it’s also the neurotransmitter of memory, attention, and connection. Maybe the real problem isn’t the drug-it’s that we’ve forgotten how to listen to our bodies before we reach for a pill.
neeraj maor
They’re lying. This whole "anticholinergic burden" thing is a cover. The real agenda? To push you toward expensive biologics and brain-altering SSRIs. The FDA is controlled by pharma. The EHR systems are owned by corporations. They want you dependent on their ecosystem. Peppermint oil? Too cheap. Too natural. Can’t patent it. So they scare you into switching to something that costs $400 a month.
Ritwik Bose
Thank you for sharing this vital information 🙏 In India, we often rely on Ayurvedic remedies like ajwain water and yoga for IBS, which are gentle and holistic. However, I understand many in the West are unaware of these options. I hope this awareness spreads globally. Let us combine wisdom from all traditions for better health.
Michael Marchio
You think mirabegron is safe? It’s a beta-3 agonist-it’s literally a synthetic stimulant for your bladder. You think your heart doesn’t feel that? I’ve seen patients with atrial fibrillation after switching. You’re trading one risk for another. There’s no perfect solution. Just less bad ones.






Write a comment