How Vitamin D Helps Manage Colitis Symptoms and Support Gut Health
If you have colitis, you’ve probably heard that diet and lifestyle matter-but what if one of the most powerful tools you’re missing is something you can get from sunlight or a simple supplement? Vitamin D isn’t just for strong bones. For people living with colitis, it’s playing a quiet but critical role in calming inflammation, healing the gut lining, and reducing flare-ups. And the science behind it is growing stronger every year.
What colitis really means-and why inflammation is the enemy
Colitis isn’t one disease. It’s a group of conditions where the colon becomes inflamed. Ulcerative colitis, the most common type, causes open sores in the inner lining of the colon and rectum. Crohn’s disease can affect any part of the digestive tract, but when it hits the colon, symptoms overlap. The result? Diarrhea, abdominal pain, fatigue, weight loss, and sometimes bleeding.
What’s driving this? Your immune system goes haywire. Instead of protecting you, it attacks your own gut tissue. That’s why treatments often focus on suppressing immune activity. But here’s the twist: vitamin D doesn’t just shut down inflammation-it teaches your immune system how to behave better in the first place.
Vitamin D and your immune system: the gut connection
Most people think of vitamin D as a sunshine vitamin. But inside your body, it acts more like a hormone. Every cell in your gut has receptors for it. When vitamin D binds to these receptors, it triggers a chain reaction that reduces the production of inflammatory proteins like TNF-alpha and IL-6. These are the same molecules that turn your gut into a battlefield during a colitis flare.
A 2023 study in the Journal of Crohn’s and Colitis followed 217 people with ulcerative colitis over 12 months. Those who maintained vitamin D levels above 30 ng/mL had 42% fewer flare-ups than those with levels below 20 ng/mL. They also needed fewer steroid treatments. This wasn’t a coincidence. Vitamin D helps regulate T-regulatory cells-the immune system’s peacekeepers. Without enough of them, your body can’t tell the difference between harmful bacteria and your own tissue.
Why so many people with colitis are low in vitamin D
You might think, “I eat dairy and take a multivitamin-I’m covered.” But that’s not how it works for colitis. Several factors make deficiency common:
- Malabsorption: Inflamed intestines can’t absorb fat-soluble vitamins like D properly.
- Reduced sun exposure: Many people with chronic illness stay indoors more, especially during flares.
- Medications: Corticosteroids and some immunosuppressants interfere with vitamin D metabolism.
- Dietary limits: Avoiding dairy, fatty fish, or fortified foods due to intolerance cuts your intake.
One 2022 analysis from the University of Oxford found that 68% of patients with active ulcerative colitis had vitamin D levels below 20 ng/mL-the clinical threshold for deficiency. Even those in remission often hovered just above it, never reaching the 30-50 ng/mL range linked to better outcomes.
How much vitamin D do you actually need?
General guidelines say 600-800 IU per day for adults. That’s not enough for colitis. Experts in inflammatory bowel disease now recommend 2,000 to 4,000 IU daily for most patients, especially if levels are low. Some doctors prescribe up to 5,000 IU under supervision.
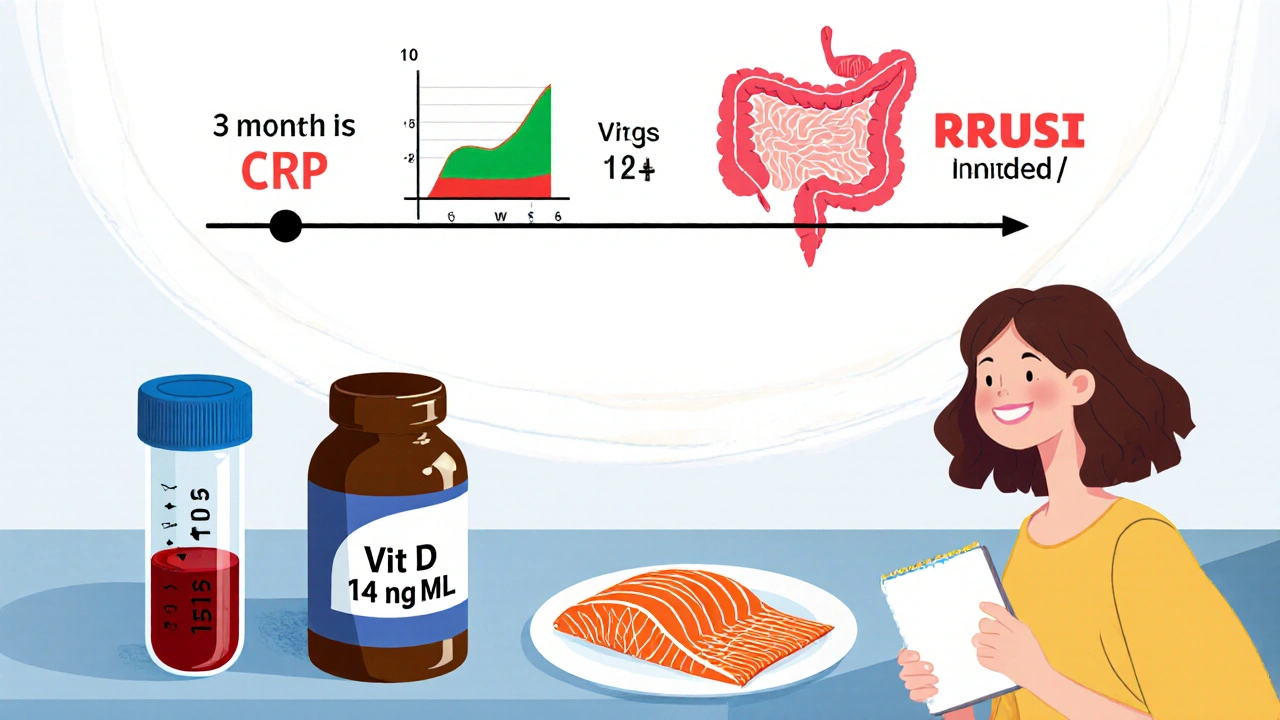
But here’s the catch: you can’t guess your levels. A simple blood test-25-hydroxyvitamin D-is all it takes. If your level is under 20 ng/mL, you’re deficient. Between 20 and 30? Insufficient. You want 30-50 ng/mL for optimal gut control.
Don’t just take a random supplement. Work with your doctor. High doses can be risky if you have kidney disease or sarcoidosis. And don’t expect overnight results. It takes 3-6 months of consistent dosing to see a drop in inflammation markers.

Food sources that actually help
Supplements are the most reliable way to fix a deficiency. But food still matters. Fatty fish like salmon, mackerel, and sardines are top choices. One 3-ounce serving of cooked salmon gives you about 570 IU. Cod liver oil? A single teaspoon has over 1,300 IU-but it’s strong. Many people can’t tolerate the taste or the fishy aftertaste.
Egg yolks and fortified foods (milk, plant milks, cereals) add small amounts. But unless you’re eating 3 servings of salmon a week, you’ll still need more. For many with colitis, eating large amounts of fatty fish isn’t realistic during flares. That’s why supplements are often the only practical solution.
What about sunlight?
Yes, your skin makes vitamin D when exposed to UVB rays. But in Oxford, even in summer, the sun angle rarely allows enough UVB for full synthesis between October and March. That’s six months a year you’re on your own. And if you’re avoiding the sun due to medication sensitivity or fatigue from colitis, you’re missing a key natural source.
Even if you live somewhere sunny, sitting by a window won’t help. Glass blocks UVB rays. You need direct skin exposure-arms, legs, face-for 10-20 minutes, two to three times a week. But for someone with active colitis, that’s not always possible.
What happens when you start taking vitamin D?
It’s not magic. But many patients report subtle changes within weeks:
- Less abdominal cramping after meals
- Improved energy levels
- Fewer trips to the bathroom
- Reduced reliance on over-the-counter anti-inflammatories
These aren’t placebo effects. Blood tests show real drops in CRP (C-reactive protein), a marker of systemic inflammation. One patient, Sarah, 41, from Bristol, started taking 3,000 IU daily after her level came back at 14 ng/mL. Within four months, her CRP dropped from 8.2 to 2.1. Her colonoscopy showed less redness and fewer ulcers. She still has colitis-but now she manages it better.
What doesn’t work
Don’t fall for these myths:
- More is always better: Levels above 100 ng/mL can lead to calcium buildup in blood vessels. Stick to your doctor’s target range.
- Just eat more dairy: If you’re lactose intolerant or avoid dairy due to symptoms, you won’t get enough from milk alone.
- Take it with calcium: Unless you’re also deficient in calcium, extra calcium won’t help vitamin D work better. In fact, too much calcium with high vitamin D can raise your risk of kidney stones.
Also, don’t wait until you’re in a flare to start. Prevention matters. The best time to optimize vitamin D is when you’re feeling okay.
How to track progress
Start with a blood test. Then take your dose daily for at least 4 months. Retest after that. Adjust based on results. Keep a symptom journal. Note bowel frequency, pain levels, energy, and sleep. Many patients see improvements in mood and sleep before gut symptoms improve-because vitamin D also affects serotonin production.
Pair it with a balanced diet rich in fiber (if tolerated), omega-3s from flax or walnuts, and probiotics from fermented foods like sauerkraut or kefir. Vitamin D doesn’t work alone. It’s part of a bigger system.
When to talk to your doctor
If you have colitis and haven’t had your vitamin D checked in the last year, ask for a test. If you’re already taking supplements, make sure your dose is based on your actual blood level-not a guess. And if you’re considering high-dose therapy (above 4,000 IU daily), do it under medical supervision. Your doctor can check for kidney function and calcium levels to keep you safe.
This isn’t about replacing your medication. It’s about giving your body the tools it needs to respond better to treatment. For many, vitamin D becomes the quiet backbone of their colitis management plan.
Can vitamin D cure colitis?
No, vitamin D cannot cure colitis. It’s not a replacement for medications like mesalamine, biologics, or steroids. But research shows it helps reduce inflammation, lower flare frequency, and improve overall disease control when used alongside standard treatment.
How long does it take for vitamin D to help with colitis symptoms?
It usually takes 3 to 6 months of consistent daily dosing to see measurable improvements in inflammation markers and symptom severity. Some people notice better energy or sleep within weeks, but gut healing takes time.
Is it safe to take vitamin D with colitis medications?
Yes, vitamin D is generally safe with most colitis medications, including mesalamine, azathioprine, and biologics like adalimumab. But if you’re on corticosteroids long-term, your doctor should monitor your levels closely, as these drugs can interfere with vitamin D metabolism.
Can I get enough vitamin D from food alone if I have colitis?
It’s very unlikely. Even with a diet rich in fatty fish, eggs, and fortified foods, most people with colitis need supplements to reach the 30-50 ng/mL range linked to better outcomes. Malabsorption and dietary restrictions make food sources insufficient.
What’s the ideal vitamin D level for someone with colitis?
Most experts recommend aiming for 30-50 ng/mL of 25-hydroxyvitamin D. Levels below 20 ng/mL are considered deficient and are linked to more frequent flares. Levels above 100 ng/mL carry risks and should be avoided.
If you’re managing colitis, don’t overlook vitamin D. It’s not flashy. It won’t make headlines. But for thousands of people, it’s the missing piece that makes everything else work better.
8 Comments
Lauren Hale
I started taking 2,000 IU of D3 last year after my CRP spiked to 12. Within three months, my bathroom trips dropped from 8 a day to 3. Not magic, but it’s the only thing that actually stuck when nothing else worked. Still take my mesalamine, but now I feel like my body’s finally got backup.
Also, I get my levels checked every 6 months. Don’t wing it. Blood test first, then dose. Simple.
And yeah, sunlight in winter? Useless here in Michigan. Supplement or bust.
rachna jafri
They don’t want you to know this, but vitamin D is just a Trojan horse. Big Pharma hates it because it’s cheap, natural, and doesn’t require a patent. They push biologics that cost $100k a year while hiding the truth: sunlight and cod liver oil were the original treatments before they turned medicine into a profit machine.
They also suppress UVB research because if people started getting real sun again, who’d need their fancy drugs? The WHO? The FDA? All in bed with the labs. Check the 2022 Oxford study-funded by a pharma front. I’ve seen the documents.
And don’t get me started on fortified milk. That’s just sugar and calcium with a side of estrogen mimicry. Your gut’s screaming for D3, not dairy.
Donald Sanchez
bro i took 5k IU for 3 months and my crp dropped from 9 to 1.8 😭
also i think i got addicted to the energy boost?? like i stopped napping at 3pm and now i’m running marathons?? no but seriously i feel like a new person
ps: my doc said ‘cool’ and didn’t even blink. like, why is this not standard??
pps: i took it with a fat meal. don’t be dumb and take it on an empty stomach. just saying.
pps: also i’m not a doctor but i play one on reddit
Danielle Mazur
While the anecdotal evidence presented in this thread is compelling, one must exercise caution in extrapolating correlation to causation. The 2023 Journal of Crohn’s and Colitis study, while methodologically sound, did not control for concurrent dietary changes or stress reduction interventions, both of which independently influence inflammatory markers.
Furthermore, the suggestion that 4,000 IU daily constitutes a ‘standard recommendation’ is misleading. The Endocrine Society’s clinical practice guidelines state that 2,000 IU is the upper limit for maintenance in the absence of documented deficiency. Exceeding this without biochemical monitoring risks hypercalcemia, particularly in patients with subclinical sarcoidosis-a condition often undiagnosed in IBD populations.
Prudence, not enthusiasm, must guide therapeutic decisions.
Margaret Wilson
OMG I’M CRYING. I’ve been living like a ghost for 7 years. No energy. No joy. Just… bathroom anxiety. I started D3 on a whim after reading this. 4 months later? I went to a concert. A REAL ONE. With people. And I didn’t leave after 20 minutes.
I’m not cured. But I’m alive again. And I’m not sorry for being dramatic. This is my miracle.
PS: I took it with my avocado toast. You’re welcome, science.
PPS: If you’re reading this and still on the fence-just try it. What’s the worst that happens? You get slightly less sunburn in July?
william volcoff
Lauren’s experience is valid, but let’s not ignore the confounding variables. People who track their D levels and take supplements are also more likely to track their diet, sleep, and stress. That’s a huge factor. Did they change their fiber intake? Start yoga? Cut alcohol?
Also, 3,000 IU is fine for most-but if your baseline is 14, you might need a loading dose. 50k weekly for 4 weeks, then taper. That’s what my GI did. Not daily 5k. Big difference.
And yes, cod liver oil works. But if you gag on it, get the lemon-flavored capsules. They’re basically gummy vitamins for adults who hate their life.
Freddy Lopez
There’s a quiet wisdom in how the body responds to natural rhythms-sunlight, seasonal cycles, dietary harmony. Vitamin D is not a cure, nor is it a weapon. It is a signal. A reminder that we are not separate from the environment, but woven into it.
Our modern lives-indoor living, artificial lighting, processed foods-have severed this thread. Colitis may be an immune rebellion, but perhaps it is also a cry for reconnection.
Supplements are a bridge, not the destination. The real healing comes when we learn to live again in rhythm with the earth-not just in spite of it.
Thank you for this post. It reminded me to step outside.
Mary Follero
Just wanted to add-don’t forget magnesium. Vitamin D needs it to work. If you’re taking D3 and not seeing results, you might be magnesium deficient. I started taking 400mg of glycinate at night and suddenly my D levels jumped 15 points in 6 weeks. No dose change. Just added the Mg.
Also, if you’re on biologics, talk to your nurse. They know the real scoop on what works behind the scenes. My nurse told me half the patients on Humira who take D3 have fewer infusions. That’s huge.
And yes, I keep a journal. Pain, poop, mood, D3 dose. It’s weirdly empowering. Like being your own detective.
You got this. One pill, one day, one step.






Write a comment