Provider Education: Understanding Biosimilar Differences
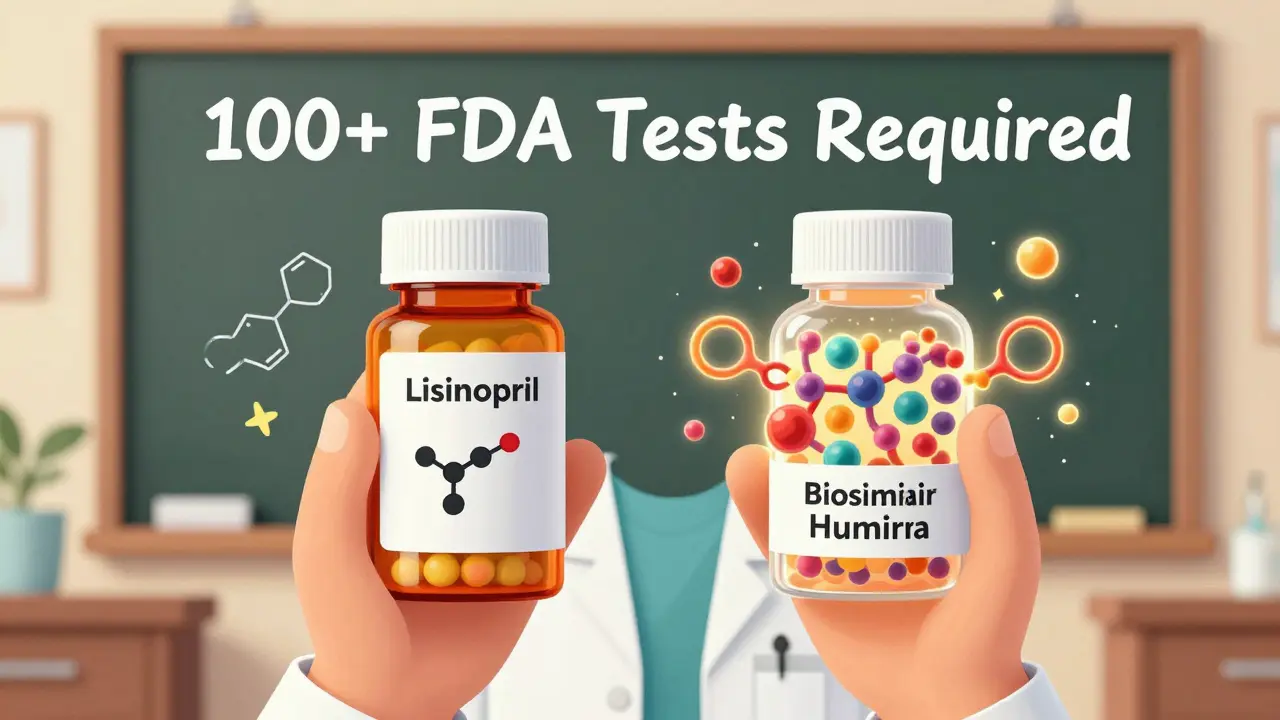
When a patient walks into your clinic with a prescription for a biologic drug like Humira or Enbrel, you might assume the generic version is just around the corner. But if you reach for the same script you’d use for a pill like lisinopril, you’re missing a critical distinction. Biosimilars aren’t generics. They’re not even close.
Think of it this way: a generic drug is a copy of a chemical compound-simple, stable, and easy to replicate. A biosimilar is a copy of a living thing. It’s made from living cells, grown in complex bioreactors, and shaped by delicate biological processes. Even tiny changes in temperature, pH, or cell line can alter the final product. That’s why the FDA requires over 100 analytical tests just to prove a biosimilar is highly similar to the original. And even then, you can’t just swap them like you would with a pill.
Here’s the real problem: most providers still don’t get it. A 2021 survey found only 38% of U.S. physicians felt extremely familiar with the FDA’s definition of a biosimilar. That’s not just a knowledge gap-it’s a patient safety risk. When a rheumatologist switches a patient from reference infliximab to a biosimilar without understanding immunogenicity risks, or when a pharmacist substitutes an interchangeable biosimilar without checking state laws, the consequences can ripple through care.
What Exactly Makes a Biosimilar Different from a Generic?
Generics are chemically identical to their brand-name counterparts. They have the same active ingredient, same molecular structure, same dosage form. You can synthesize them in a lab using standard chemistry. That’s why a generic metformin tablet looks and acts exactly like Glucophage.
Biosimilars? They’re not identical. They’re highly similar. The FDA allows minor differences in inactive ingredients, glycosylation patterns, or protein folding-as long as those differences don’t affect safety or effectiveness. That’s why biosimilars need clinical trials. Not just bioequivalence studies like generics, but full Phase 1 and Phase 3 trials comparing immune responses, adverse events, and long-term outcomes against the reference product.
Take insulin glargine. The original, Lantus, was approved in 2000. By 2015, the first biosimilar, Basaglar, hit the market. It’s not the same molecule. It has a slightly different manufacturing process. But after 1,200 patients were studied across three trials, the FDA concluded there was no clinically meaningful difference. That’s the bar. And it’s way higher than the bioequivalence threshold for generics.
And here’s the kicker: biosimilars can’t be automatically substituted unless they’re designated as “interchangeable.” That’s a separate FDA classification requiring additional studies showing that switching back and forth between the reference product and the biosimilar doesn’t increase risk or reduce effectiveness. Only five biosimilars in the U.S. have that status as of late 2025. The rest require a prescriber to explicitly write “dispense as written” or risk a pharmacy refusal.
Why Do Providers Still Hesitate?
It’s not just ignorance. It’s fear. And it’s well-placed-if you’re not trained.
One major concern is extrapolation. A biosimilar might be tested only in rheumatoid arthritis, but get approved for psoriasis, Crohn’s, and ankylosing spondylitis too. That’s allowed under FDA guidelines if the mechanism of action is the same and the target tissues are similar. But many providers don’t feel comfortable prescribing for an indication they didn’t see in the trial data. A 2019 study found 57% of U.S. providers were unsure about using biosimilars for unstudied conditions.
Then there’s immunogenicity. Biologics can trigger immune responses. That’s why some patients develop neutralizing antibodies and lose response over time. Biosimilars can have slightly different immunogenic profiles. Not dangerous-just different. But if you don’t know how to monitor for it, you might misattribute a loss of efficacy to the biosimilar instead of disease progression.
And EHRs? They’re a mess. A 2022 survey of 150 U.S. hospitals found 78% had trouble tracking biosimilars in their electronic systems. Epic, Cerner, Allscripts-all were designed to treat drugs as interchangeable. No field for “biosimilar,” no flag for “reference product,” no automatic alert when a patient switches. So providers just assume the system is right. And when a patient comes back with a flare-up, no one knows if it’s the drug, the disease, or a documentation error.
Who’s Leading in Adoption-and Why?
Not every specialty is stuck in the same place.
Rheumatologists are ahead. Why? Because they’ve seen the data. The American College of Rheumatology issued strong guidelines in 2021 based on 37 clinical trials involving over 12,500 patients. They’ve trained their teams. They’ve updated their protocols. And now, 68% of rheumatologists routinely prescribe biosimilars.
Oncologists are catching up. In 2017, only 12% of oncology practices used biosimilars. By 2022, that jumped to 52%. The turning point? A program at UCSF Medical Center where pharmacists ran monthly educational sessions for nurses and doctors. They showed real-world cost savings, reviewed case studies of patients who switched without issue, and even built custom EHR templates. Within six months, prescribing hesitancy dropped from 58% to 12%.
Endocrinologists? Still behind. Only 29% use insulin biosimilars, even though they’ve been available since 2015. Why? Lack of awareness. Many still think biosimilars are “new” or “untested.” But insulin glargine biosimilars have been used safely in Europe for over a decade. The data is solid. The problem isn’t the science-it’s the education.
What Providers Need to Know-And When
If you’re going to prescribe or dispense biosimilars, here’s what you need to master:
- Regulatory status: Is it biosimilar? Or interchangeable? Only interchangeable products can be substituted at the pharmacy without prescriber approval-and only in states that allow it. As of 2025, 42 U.S. states have substitution laws, but notification rules vary. Some require immediate notice. Others give 7 days. Six states don’t require any.
- Indication extrapolation: Just because a biosimilar was tested in one condition doesn’t mean it’s unsafe in others. But you should understand the scientific rationale. The FDA requires demonstration of similar mechanism of action, target binding, and pharmacokinetics across conditions.
- Immunogenicity monitoring: Track response over time. If a patient loses efficacy after switching, don’t assume it’s the biosimilar. Check antibody levels, review dosing, assess disease activity. Sometimes, it’s just a need for a dose adjustment.
- EHR documentation: Make sure your system can distinguish between reference product and biosimilar. If it can’t, push for a fix. Otherwise, you’re flying blind.
- Cost and reimbursement: Medicare Part B pays 28% less for biosimilars than reference biologics in 2022 data. That’s real savings. But billing codes are tricky. Some payers still use the same code for both. Others require a modifier. Know your payer rules.

Where to Get Reliable Education
You don’t need to dig through 50 journal articles. The FDA has already done the work.
The Office of Therapeutic Biologics and Biosimilars (OTBB) offers a free, comprehensive Teaching Resource Guide with 12 modules. It covers everything from manufacturing to interchangeability to real-world evidence. All materials are available in nine languages and meet Section 508 accessibility standards. No login. No cost. Just go to fda.gov/biosimilars/education.
Professional societies are stepping up too. The Arthritis Foundation launched a provider education campaign in early 2023. Over 12,500 clinicians accessed their resources in six months. The American Society of Health-System Pharmacists (ASHP) has a biosimilar toolkit for pharmacists. The Alliance for Safe Biologic Medicines offers free webinars and case studies.
And don’t underestimate the power of your own pharmacy team. A 2022 survey found 76% of hospitals now rely on clinical pharmacists to lead biosimilar education. They’re the ones who know the billing codes, the EHR quirks, and the patient counseling points.
What’s Next?
The market is growing fast. Global biosimilar sales hit $12.3 billion in 2022 and are projected to reach $45 billion by 2027. By 2025, the Association of American Medical Colleges plans to integrate biosimilar education into 95% of medical school curricula. The FDA’s 2024 update will include more real-world data-exactly what 73% of providers say they need.
But progress depends on you. If you’re still unsure whether biosimilars are safe, you’re not alone. But you’re also behind. The data is there. The tools are free. The patients are waiting.
Don’t wait for someone else to educate you. Start today. Read one module. Talk to your pharmacist. Ask your EHR vendor for a biosimilar flag. Your patients will thank you-with better access, lower costs, and no loss of effectiveness.
Are biosimilars the same as generics?
No. Generics are chemically identical copies of small-molecule drugs. Biosimilars are highly similar copies of complex biologic drugs made from living cells. They require extensive clinical testing to prove safety and effectiveness, while generics only need bioequivalence studies.
Can any biosimilar be automatically substituted at the pharmacy?
Only if it’s designated as “interchangeable” by the FDA and your state allows substitution. As of 2025, only five biosimilars in the U.S. have interchangeability status. Even then, 6 states don’t require any prescriber notification, while others require 7-day notice. Always check your state’s law.
Why are biosimilars cheaper if they’re so complex to make?
Because they don’t need to repeat the full clinical development program. The manufacturer can rely on the reference product’s safety and efficacy data, cutting years off development time and billions off R&D costs. That’s why they’re priced 15-30% lower, even though manufacturing is more expensive than making a pill.
Do biosimilars have the same side effects as the original biologic?
They have the same types of side effects, but rates may vary slightly due to differences in manufacturing. These differences are not clinically meaningful. Studies show no increase in serious adverse events, immunogenicity, or loss of efficacy when switching from reference product to biosimilar.
What should I do if a patient is nervous about switching to a biosimilar?
Listen first. Then explain: biosimilars are not experimental. They’ve been used safely in Europe for over 15 years and in the U.S. since 2015. Show them the FDA’s approval process. Share data from studies showing no difference in outcomes. And make sure your EHR documents the switch clearly so future providers know what was given.
Is there evidence that biosimilars work in real-world settings?
Yes. Real-world studies from the U.S., Europe, and Canada show equivalent effectiveness and safety for conditions like rheumatoid arthritis, Crohn’s disease, and certain cancers. For example, a 2023 study of 11,000 patients switching from reference infliximab to a biosimilar found no increase in disease flares or hospitalizations over 24 months.
How can I improve biosimilar adoption in my practice?
Start with education: use the FDA’s free Teaching Resource Guide. Partner with your pharmacy team to build a simple workflow. Update your EHR to track biosimilars separately. Train your staff on counseling points. And begin with one condition-like rheumatoid arthritis-where data is strongest. Success there builds confidence for broader use.
Providers who take the time to understand biosimilars don’t just save money-they unlock access to life-changing therapies for patients who otherwise couldn’t afford them. The science is clear. The tools are ready. The only thing missing is action.
15 Comments
Anu radha
I just switched my mom to a biosimilar for her arthritis last month. She’s been fine-no flare-ups, no weird side effects. Honestly, I was scared too, but now I wish we’d done it sooner. Money saved means she can get her physical therapy sessions without skipping weeks.
Jigar shah
The distinction between generics and biosimilars is fundamentally rooted in molecular complexity. While generics are small-molecule compounds with well-defined synthesis pathways, biosimilars are large, glycosylated proteins produced via live-cell fermentation, introducing inherent heterogeneity. The FDA’s requirement for comparative clinical trials reflects this biological nuance, not regulatory overreach.
Naomi Lopez
Ugh, I can’t believe we’re still having this conversation in 2025. Biosimilars are basically the pharmaceutical industry’s way of saying ‘we’re bored of charging $20k a year for Humira.’ If you’re still scared of them, maybe you should’ve gone into accounting instead of medicine.
Salome Perez
What a beautifully written piece-thank you for making such a complex topic feel accessible. I’ve shared this with my entire clinic team, and we’ve already started using the FDA’s Teaching Resource Guide in our monthly huddles. One of our nurses, who used to dread biosimilar conversations, now leads patient education sessions. It’s amazing what clarity can do. The real win? Patients feel heard, not just prescribed to.
Victoria Rogers
Why do we even let foreign-made biosimilars in? The US makes the best drugs. These cheap knockoffs are just a Trojan horse for global supply chain chaos. One day, a patient’s insulin will fail because some factory in Bangalore had a power outage. And you’ll blame the doctor. Not the system.
Jane Wei
My rheumatologist switched me last year. Felt the same. Paid half. No drama. Why is this even a thing?
Jody Patrick
My cousin in Delhi got her biosimilar insulin last year. Cost was one-tenth of the brand. She’s been stable for 18 months. We don’t need fancy studies-real people are living better because of this. Education just needs to reach the clinics, not just the big hospitals.
Philippa Skiadopoulou
The regulatory framework for biosimilars is robust and evidence-based. The key challenge lies not in science but in communication. Providers must be equipped to articulate the distinction between ‘identical’ and ‘highly similar’ to patients without inducing unnecessary anxiety. Clarity, not jargon, is the goal.
Pawan Chaudhary
This is the kind of info that gives me hope. We’ve been stuck in the dark for too long. If even one doc reads this and changes how they talk to a patient, that’s a win. Keep sharing stuff like this. We need more of it.
Peter Ronai
Let’s be real-this whole biosimilar push is a pharma scam. They don’t care about patients. They care about patent cliffs. The FDA’s ‘highly similar’ is just corporate speak for ‘close enough to get paid.’ And don’t get me started on the 78% of EHRs that can’t track them. That’s not incompetence-that’s collusion.
Steven Lavoie
As someone who works in global health, I’ve seen biosimilars change lives in low-resource settings. In Kenya, a patient on a biosimilar infliximab is now able to work again. In rural Alabama, a single mom can afford her daughter’s biologic. This isn’t about cost-cutting. It’s about justice. The science is sound. The ethics are clear. The resistance? That’s the real problem.
Martin Spedding
LOL biosimilars. You think you’re saving money? Wait till the first lawsuit when some kid gets a rare autoimmune reaction because the glycosylation was off by 0.3%. Then we’ll see who’s laughing. And no, the FDA doesn’t ‘prove’ safety-they just approve based on corporate data. Wake up.
amanda s
Why are we letting China and India make our life-saving drugs? This isn’t healthcare-it’s national security breach. If your kid needs insulin, you better hope their biosimilar came from a US plant. Otherwise, you’re gambling with their life. And your doctor? They’re just following orders from Big Pharma’s playbook.
Jonathan Morris
Ever wonder why the FDA approves biosimilars so fast? They’re not testing for safety-they’re testing for corporate compliance. The real data? Buried in proprietary databases. The 100+ tests? Just paperwork. Real-world outcomes? Ignored. This is how you get a system that kills people quietly while calling it ‘innovation.’
Victoria Rogers
Oh so now you’re telling me the EHRs are broken? That’s the whole point. They’re designed to keep you confused. If your system can’t tell the difference between Humira and its biosimilar, you’re not supposed to notice. That’s how they keep you dependent on the brand.






Write a comment