How to Know If Your Supplement Is Safe with Your Medications

More than three in four adults in the U.S. take dietary supplements. Many believe these are harmless because they’re labeled “natural.” But here’s the truth: supplement and medication interactions send about 23,000 people to the emergency room every year. That’s not a small risk. It’s a quiet, widespread danger - one you might not even realize you’re facing.
Why Supplements Aren’t Always Safe with Medications
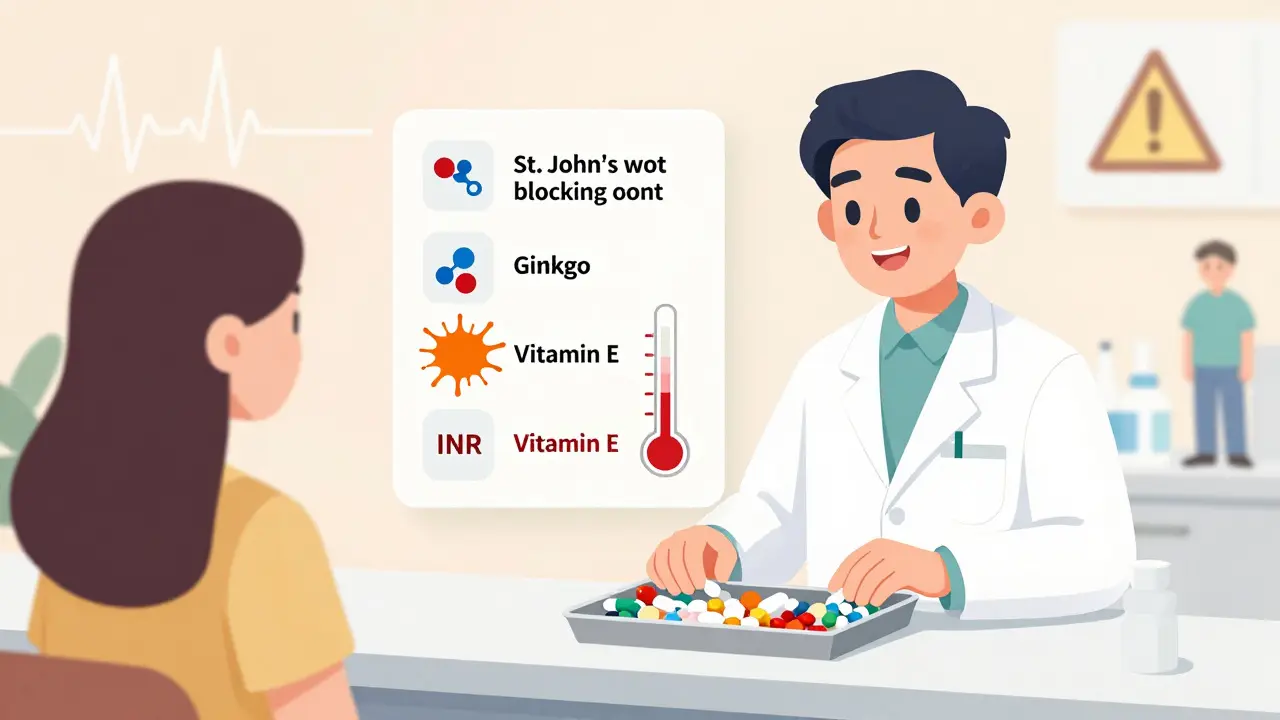
Supplements don’t go through the same safety tests as prescription drugs. Under the 1994 Dietary Supplement Health and Education Act, manufacturers don’t need to prove their products are safe before selling them. That means a bottle of ginkgo biloba or fish oil might look harmless - but it could be quietly interfering with your blood thinner, antidepressant, or heart medication. The real problem lies in how your body processes both drugs and supplements. Many of them are broken down by the same liver enzymes - especially the CYP3A4 and CYP2C9 systems. When a supplement blocks or speeds up these enzymes, your medication either builds up to toxic levels or gets flushed out too fast. For example, St. John’s wort can reduce the effectiveness of cyclosporine - a drug transplant patients rely on - by up to 50%. That’s not a minor drop. It’s a life-threatening one.The Top 3 Dangerous Supplements and What They Do
Not all supplements are created equal when it comes to risk. Some are mostly harmless. Others are ticking time bombs when mixed with common meds.- St. John’s wort: This popular herb for mild depression interacts with over 57 prescription drugs. It can make birth control fail, reduce the power of HIV meds, and blunt the effect of antidepressants like SSRIs - sometimes triggering serotonin syndrome, a potentially fatal condition. The FDA has warned about this since 2006, and it’s still the #1 offender.
- Ginkgo biloba: Often taken for memory or circulation, ginkgo thins the blood. When paired with warfarin, Eliquis, or aspirin, it can cause serious bleeding. One study found it triples the risk of major bleeding in people on blood thinners. A Reddit user reported a 7-day hospital stay after combining ginkgo with Eliquis - a real case, not a hypothetical.
- Vitamin E (400 IU or more): High doses boost bleeding risk in people taking warfarin. Studies show it can raise INR levels by 15-20%, pushing patients into dangerous territory where even a minor cut won’t stop bleeding.
What’s Actually Safe (and What’s Not)
You don’t have to give up all supplements. Some have minimal interaction risk. According to the American Academy of Family Physicians, these are generally low-risk: milk thistle, cranberry, American ginseng, saw palmetto, and valerian. But “generally” doesn’t mean “always.” Even milk thistle has been linked to rare interactions with drugs processed by CYP2C9. Here’s the catch: if you’re on a medication with a narrow therapeutic index - meaning the difference between a helpful dose and a toxic one is tiny - you need to be extra careful. These include:- Warfarin (Coumadin)
- Digoxin
- Cyclosporine
- Levothyroxine
- Phenytoin
How to Check for Interactions - Step by Step
You don’t need a pharmacy degree to protect yourself. Here’s what actually works:- Make a complete list. Write down every prescription, over-the-counter drug, vitamin, herb, and mineral you take - including the dose and how often. Don’t forget things like magnesium for sleep or turmeric capsules for joint pain.
- Use the brown bag method. Once a year, or before any surgery, bring all your meds and supplements to your pharmacist or doctor. Put them in a brown paper bag and say, “Can you check these together?” This simple step, proven in a Johns Hopkins study, cuts medication errors by 37%.
- Ask about interactions. Don’t say, “Is this safe?” Say, “I’m taking [medication]. I’m also taking [supplement]. Could they affect each other?” Pharmacists are trained for this. In 2021, Walgreens started requiring staff to screen for supplement interactions - and found dangerous combos in 18% of cases.
- Check the label. Look for warning statements. If it says “May interact with blood thinners” or “Do not use with antidepressants,” take it seriously. Many brands now include this - but not all.
Who’s at Highest Risk - And Why Nobody Tells You
People over 50 are the most vulnerable. About 78% in this group take both prescription meds and supplements. Yet only 32% talk to their doctor about it. Why? Because they think “natural” means “safe.” A 2023 survey found 41% of supplement users believe they don’t need to mention them to their provider. Doctors aren’t always to blame either. Until June 2023, the American Medical Association didn’t require them to ask about supplements during medication reviews. That changed. Now, they’re supposed to. But many still don’t. You have to be the one to start the conversation.
What’s Changing - And What’s Coming
The tide is turning. In March 2024, the FDA announced a new mobile app - the Dietary Supplement Ingredient Database - that will let you scan a supplement label and instantly see interaction risks. It’s set to launch in late 2024. That’s a game-changer. Meanwhile, Epic Systems - the company behind most U.S. hospital electronic records - has started adding supplement interaction alerts to patient charts. Right now, it’s only in 15% of hospitals. But that number is rising. The FDA is also cracking down harder. In 2023, they issued 142 warning letters to companies making illegal drug claims on supplements - like saying their product “replaces statins” or “cures diabetes.” These aren’t just misleading. They’re deadly.What to Do Right Now
Don’t wait for the app. Don’t wait for your doctor to ask. Take action today:- Stop assuming “natural” = safe. It doesn’t.
- Check your supplements against your prescriptions. Use a free tool like Drugs.com’s interaction checker - but treat it as a starting point, not the final word.
- Call your pharmacist. They’re paid to catch these things. And they’re often more up-to-date than your doctor on supplement risks.
- If you’re scheduled for surgery, stop ginkgo, garlic, fish oil, and vitamin E at least 7-10 days before. Your surgeon will thank you.
- Keep your list updated. Add new supplements as soon as you start them. Delete ones you stop.
Final Thought: You’re the Last Line of Defense
No one is watching out for you like you can. Regulators are slow. Doctors are busy. Pharmacies are understaffed. But you have your list. You have your bottles. You have your life. Supplements aren’t the enemy. But pretending they’re harmless while you’re on prescription meds? That’s the real danger. Start today. Pull out your brown bag. Talk to your pharmacist. Ask the question: “Could this hurt me?” It’s not paranoia. It’s protection.Can I take vitamin D with my blood pressure medication?
Yes, vitamin D is generally safe with most blood pressure medications. There’s no strong evidence it interferes with ACE inhibitors, beta-blockers, or calcium channel blockers. But if you’re taking a thiazide diuretic (like hydrochlorothiazide), high doses of vitamin D can raise calcium levels too much - which might affect your heart rhythm. Stick to 1,000-2,000 IU daily unless your doctor says otherwise.
Is it safe to take magnesium with my heart medication?
It depends. Magnesium can interfere with certain antibiotics like tetracycline and quinolones, and it may reduce the absorption of thyroid meds like levothyroxine. But for heart patients on digoxin, magnesium can actually help prevent dangerous rhythms. If you’re on a beta-blocker or calcium channel blocker, magnesium is usually fine. Just take it at least 2 hours apart from other meds to avoid absorption issues.
Can St. John’s wort make my birth control fail?
Yes. St. John’s wort speeds up how your body breaks down estrogen and progestin. This can drop hormone levels enough to cause ovulation - even if you’re taking your pill every day. Over 280 users on Drugs.com reported unintended pregnancies after combining the two. If you’re using hormonal birth control, avoid St. John’s wort completely.
What supplements should I avoid before surgery?
Stop these at least 7-10 days before any surgery: ginkgo biloba, garlic, fish oil, vitamin E (400 IU+), ginger, and green tea extract. All can increase bleeding risk. Even turmeric - often thought of as safe - can thin the blood. Your surgeon’s office should give you a list, but don’t assume they know about every supplement you take. Bring your brown bag.
Are there any supplements that help with medication side effects?
Some can - but only under supervision. Coenzyme Q10 is sometimes used with statins to help with muscle pain, though evidence is mixed. Probiotics may help with antibiotic-related diarrhea. Magnesium can ease constipation from opioids. But don’t self-prescribe. What helps one person might worsen another’s condition. Always check with your pharmacist first.
Can I trust supplement labels that say “drug-free” or “no interactions”?
No. There’s no legal requirement for supplement makers to test for drug interactions. A label saying “no interactions” is meaningless. The FDA doesn’t approve supplement labels for safety claims. Even if a product is certified by USP or NSF, that only verifies ingredients and purity - not how it reacts with your meds.
What should I do if I think a supplement is causing a problem?
Stop the supplement immediately. Contact your doctor or pharmacist. If you have symptoms like unusual bleeding, dizziness, confusion, rapid heartbeat, or severe nausea, go to urgent care. Report the issue to the FDA’s MedWatch program - it helps track dangerous combos. Your report could help prevent someone else’s hospital stay.
10 Comments
Sazzy De
Been taking fish oil and lisinopril for years never thought twice about it until I read this. Now I'm double checking everything. Good reminder that natural doesn't mean harmless.
Blair Kelly
St. John’s wort is a silent killer. I had a cousin on SSRIs take it for ‘anxiety’ and ended up in the ER with serotonin syndrome. The FDA warned about this in 2006 and people are STILL doing it. Labeling laws are a joke. If you’re on any psych med, don’t touch it. Period.
Kelly Weinhold
Love that you included the brown bag method. My grandma started doing this after her pharmacist caught her mixing warfarin with ginkgo. She didn’t even know she was taking it-thought it was just ‘memory support.’ Now she brings everything every visit. It’s saved her twice. You don’t need to be a doctor to protect yourself. Just be curious and a little stubborn.
Carolyn Whitehead
My mom took vitamin E with her blood thinner and almost bled out during a minor procedure. She didn’t tell anyone because she thought it was ‘just a supplement.’ Please don’t be like her. Talk to your pharmacist. They’re the real heroes here.
Kimberly Reker
My pharmacist asked me about my supplements during a routine refill and I realized I’d been taking turmeric capsules for months without telling anyone. He flagged it because I’m on Plavix. Turned out it was raising my bleeding risk. Now I keep a list on my phone. Best habit I’ve ever picked up. Thanks for the reminder.
Katie and Nathan Milburn
There’s a critical gap between public perception and clinical reality. Supplements are marketed as wellness tools but operate in a regulatory gray zone. The burden of safety falls entirely on the consumer. Until labeling and testing are standardized, vigilance isn’t optional-it’s survival.
Shubham Dixit
Why are we even talking about this? In India, we’ve been using turmeric, ashwagandha, and neem for centuries with no issues. Western medicine is obsessed with pharmaceutical control. You think your lab tests are the only truth? The body isn’t a chemistry set. You’re overcomplicating something natural. People in the West get sick because they over-medicate and under-trust their own biology. This article reads like fearmongering dressed as science.
My grandfather took ginkgo with blood pressure meds for 20 years. Lived to 98. You think he was worried about CYP3A4 enzymes? No. He ate right, walked daily, and trusted tradition. Maybe we should ask why the West is so afraid of natural remedies instead of blaming them.
Also, the FDA? They approved opioids for decades. They let Big Pharma push statins to healthy people. Who do you trust more-the guy who sells you a bottle of ashwagandha or the FDA that let fentanyl-laced pills flood the streets?
Don’t let fear of interaction make you forget the bigger picture: modern medicine is broken. Supplements aren’t the problem. The system is.
Rohit Kumar
Shubham’s comment reflects a deeper cultural divide. Traditional medicine isn’t about rejecting science-it’s about integrating wisdom with caution. But we can’t romanticize tradition either. Ashwagandha may have helped your grandfather, but it also inhibits CYP3A4. That’s not folklore-that’s pharmacokinetics. The real question isn’t East vs West. It’s: how do we honor ancestral knowledge without ignoring biological reality?
My grandmother used neem for skin infections. She didn’t know about bioavailability or enzyme inhibition. But she also never mixed it with immunosuppressants. That’s the key: context matters. Tradition without awareness is dangerous. Science without humility is arrogant.
We need a third way-not rejection, not blind acceptance. We need culturally informed pharmacology. Pharmacists trained in Ayurveda, herbalists who understand CYP450 systems. That’s the future. Not fear. Not nationalism. Integration.
Eliana Botelho
Okay but what if I just take one supplement and my doctor says it’s fine? Are you saying I’m a fool if I trust them? I’ve been on metformin for 8 years and take magnesium daily. My endo said it’s fine. Now you’re telling me I’m at risk? Who even are you to say what’s safe? I’m not going to stop taking magnesium because some guy on Reddit says so. My doctor knows my bloodwork. You don’t. You’re just scared of supplements because you don’t understand them.
And why is everyone so obsessed with the FDA? They banned ephedra but let sugar-filled cereals be sold as ‘healthy.’ Who’s really protecting us here? I’d rather trust my doctor than some app that scans labels and panics over everything.
Also, I’ve read this whole post and I still have no idea if I should take vitamin D with my blood pressure med. You say it’s ‘generally safe’ but then you say ‘if you’re on a diuretic’ and now I’m confused again. So what’s the answer? Just don’t take anything? That’s not helpful. That’s fear.
Jodi Olson
Supplements are not the enemy. Complacency is.






Write a comment