How to Use Patient Assistance Programs When No Generic Medication Exists

When you’re prescribed a medication and there’s no generic version available, you’re stuck with the brand-name drug-and that often means paying hundreds or even thousands of dollars each month. For many people, that’s simply not possible. But there’s a lifeline: patient assistance programs (PAPs). These programs exist specifically to help people who can’t afford brand-name drugs when no cheaper alternative exists. They’re not a secret. They’re not a myth. They’re real, functional, and used by over a million Americans every year. The problem? Most people don’t know how to use them, or they give up after the first roadblock.
Why PAPs Matter When There’s No Generic
Let’s say you have a rare autoimmune condition, and your doctor prescribes Soliris. It works. It saves your life. But it costs $500,000 a year. There’s no generic. No discount card will help. Without help, you’re forced to choose between your health and your rent. That’s not hypothetical. It’s happening right now.
PAPs were born out of necessity. In the 1980s, during the HIV/AIDS crisis, drugs like Retrovir cost more than $15,000 in today’s dollars. People were dying because they couldn’t pay. Pharmaceutical companies stepped in-not out of charity alone, but because they couldn’t ignore the human cost. Today, over 1,500 PAPs exist, mostly run by drugmakers themselves. In 2022 alone, these programs gave out $4.7 billion in aid. Seventy-eight percent of that went to patients who needed brand-name drugs with no generics.
For people without insurance, or those with high-deductible plans, PAPs can mean the difference between taking your medicine and not taking it at all. Studies show patients using PAPs for cancer drugs had 37% fewer cases of skipping doses because they couldn’t afford them. That’s not just money-it’s survival.
How PAPs Actually Work
Not all PAPs are the same. There are three main types:
- Manufacturer-sponsored (65%): Run directly by drug companies like Novartis, Gilead, or Eli Lilly. These usually cover 100% of the drug cost if you qualify.
- Foundation-sponsored (25%): Run by nonprofits like the Patient Access Network Foundation or the Chronic Disease Fund. These often help people with insurance who still can’t afford their copays.
- State-sponsored (10%): Programs like PACE in Pennsylvania or California’s RxHelp. These usually target seniors or low-income residents.
Eligibility is mostly based on income. Most programs use 400% of the Federal Poverty Level as the upper limit. In 2023, that was $60,000 for a single person. But some programs cap it at 200%-so if you make more than $30,000, you might still qualify for some help.
You’ll need:
- Proof of income (tax return, pay stubs, or a letter from your employer)
- A valid prescription
- Proof of U.S. residency
- Doctor’s signature on a form (72% of programs require this)
Processing time varies. Manufacturer programs approve applications in 7-10 business days. Foundation programs take longer-14 to 21 days-because they verify more paperwork. If you’re in a hurry, start with the drugmaker’s own program.
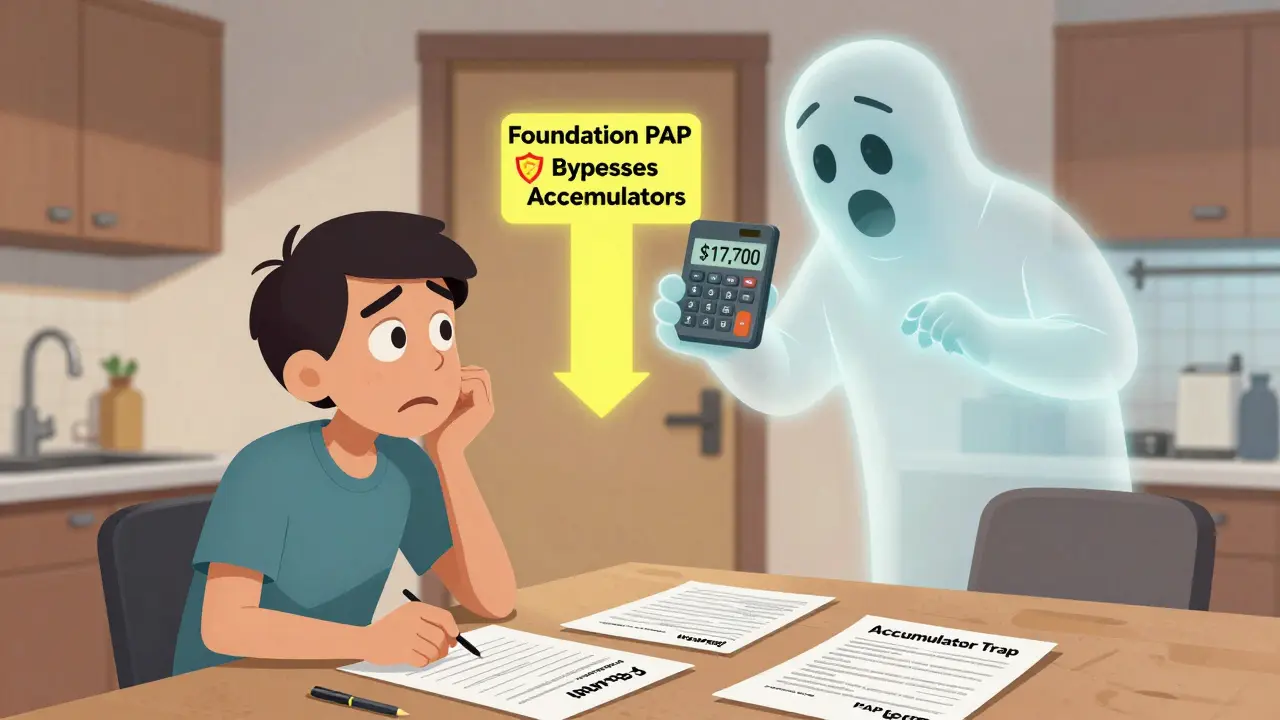
The Hidden Trap: Accumulator Adjustments
This is where most people get stuck. Even if you get approved for a PAP, your insurance might not let you use it the way you expect.
Here’s the problem: Most major pharmacy benefit managers (PBMs) like Express Scripts and Optum use something called an “accumulator adjustment.” That means the money your PAP pays toward your drug doesn’t count toward your deductible or out-of-pocket maximum. So you’re getting your medicine for free-but you’re still paying thousands out of pocket because your insurance treats you like you haven’t paid anything.
Imagine this: You’re on a $12,000-a-month cancer drug. Your PAP covers the full cost. But your deductible is $8,700. Because the PAP payment doesn’t count, you still owe $8,700. Then your out-of-pocket max is $9,000. You end up paying $17,700 in one year-even though your medicine was free. That’s not a mistake. That’s policy.
How do you avoid this? Two ways:
- Use a foundation-sponsored PAP. These aren’t subject to accumulator rules.
- Switch to a health plan that doesn’t use accumulators. Ask your insurer: “Do you have an accumulator adjustment policy?” If they say yes, consider switching during open enrollment.
And if you’re on Medicare? Forget manufacturer copay assistance. Since January 2020, Medicare rules block it. Your only option is foundation-based PAPs.
Who Can Help You Apply
You don’t have to do this alone. In fact, most successful applicants don’t.
Many hospitals now have medication access specialists-people whose job is to help patients get PAPs. These specialists handle 85% of applications at major health systems. They know which forms to fill, which documents to send, and how to chase down delays.
If your doctor’s office doesn’t have one, call your local nonprofit. Organizations like the Patient Advocate Foundation, NeedyMeds, and RxHope offer free help. Their websites have tools to screen you for eligibility in under 5 minutes. RxHope’s online screener covers 92% of manufacturer programs. Just enter your drug name, income, and insurance status. It tells you exactly which programs you qualify for-and links you to the application.
Some people try to do it themselves. That’s fine-but be ready. The average application takes 45 minutes of your time, and 17 pieces of information. If you’re missing one document, it gets rejected. And 38% of applications are rejected for incomplete paperwork. That’s why having help cuts your success rate from 52% to 81%.
Real Stories, Real Outcomes
One woman in Ohio had chronic myeloid leukemia. Her drug, Tasigna, cost $14,000 a month. She had insurance, but her copay was $1,400. She couldn’t afford it. She applied to Novartis’s PAP. Took three weeks. Submitted six documents. Got approved. Her out-of-pocket cost dropped to $0. She kept her job. She kept her treatment.
Another man in Texas had HIV. His medication cost $15,000 a month. He was uninsured. He found Gilead’s Advancing Access program. Applied online. Got approved in 8 days. His medication arrived by mail. He didn’t lose his apartment. He didn’t go without.
But then there’s the other side. A woman in Florida had a PAP approved for her $12,000-a-month cancer drug. But her insurer had an accumulator policy. She paid $20,700 out of pocket before her deductible was met. She went into debt. She nearly stopped taking her medicine.
The difference? Knowledge. She didn’t know about accumulators. She didn’t ask. She assumed the PAP meant she was done paying.
What to Do Next
Here’s your step-by-step plan:
- Find out if your drug has a PAP. Go to NeedyMeds.org or RxHope.com. Search your drug name. If it’s listed, you’re eligible.
- Check your income. Are you under 400% of the Federal Poverty Level? If yes, you likely qualify for at least one program.
- Call your doctor’s office. Ask if they have a medication access specialist. If they do, ask them to start the application.
- Ask your insurer: “Do you have an accumulator adjustment policy?” If yes, look for a foundation PAP instead of a manufacturer one.
- Submit your application. Gather your documents: tax return, prescription, ID, doctor’s form. Don’t wait. Processing takes time.
- Follow up. If you haven’t heard back in 10 days, call. Applications get lost. You have to chase them.
If you’re on Medicare, skip manufacturer PAPs. Go straight to nonprofit foundations. Programs like the Patient Access Network Foundation and the Chronic Disease Fund still help Medicare patients.
What’s Changing in 2026
Things are moving fast. In January 2025, Medicare will fully ban manufacturer copay assistance. That means more pressure on nonprofit programs. But there’s good news too.
Eli Lilly’s “Simple Bridge” program now cuts applications from 17 steps to just 5. Approval for insulin PAPs now takes 48 hours. Epic, the biggest electronic health record system, is integrating PAP tools directly into doctors’ systems. By 2026, your doctor might be able to click a button and enroll you in a PAP before you even leave the office.
But the biggest change? Awareness. More patients are learning about PAPs. More doctors are trained to help. More insurers are being forced to disclose their accumulator policies. It’s not perfect. But it’s getting better.
Final Thought
PAPs aren’t a cure for high drug prices. They’re a bandage. But for someone who can’t afford their medicine, a bandage is everything. If you’re on a brand-name drug with no generic, don’t assume you’re out of options. You’re not. You just need to know where to look-and who to ask. Start today. One call, one form, one application can change your life.





