Hyponatremia from SSRIs: Low Sodium and Confusion Risk in Older Adults
Hyponatremia Risk Calculator
Risk Assessment
Risk Assessment Result
Why Your Antidepressant Might Be Lowering Your Sodium Levels
It’s not just about feeling better emotionally. When you start an SSRI like sertraline or citalopram, your body is doing something unexpected-holding onto too much water. And that’s not harmless. This can drop your blood sodium levels dangerously low, leading to confusion, dizziness, even seizures. It’s not rare. In people over 65, up to 1 in 6 may develop this problem within weeks of starting the medication. Most don’t know it’s even possible.
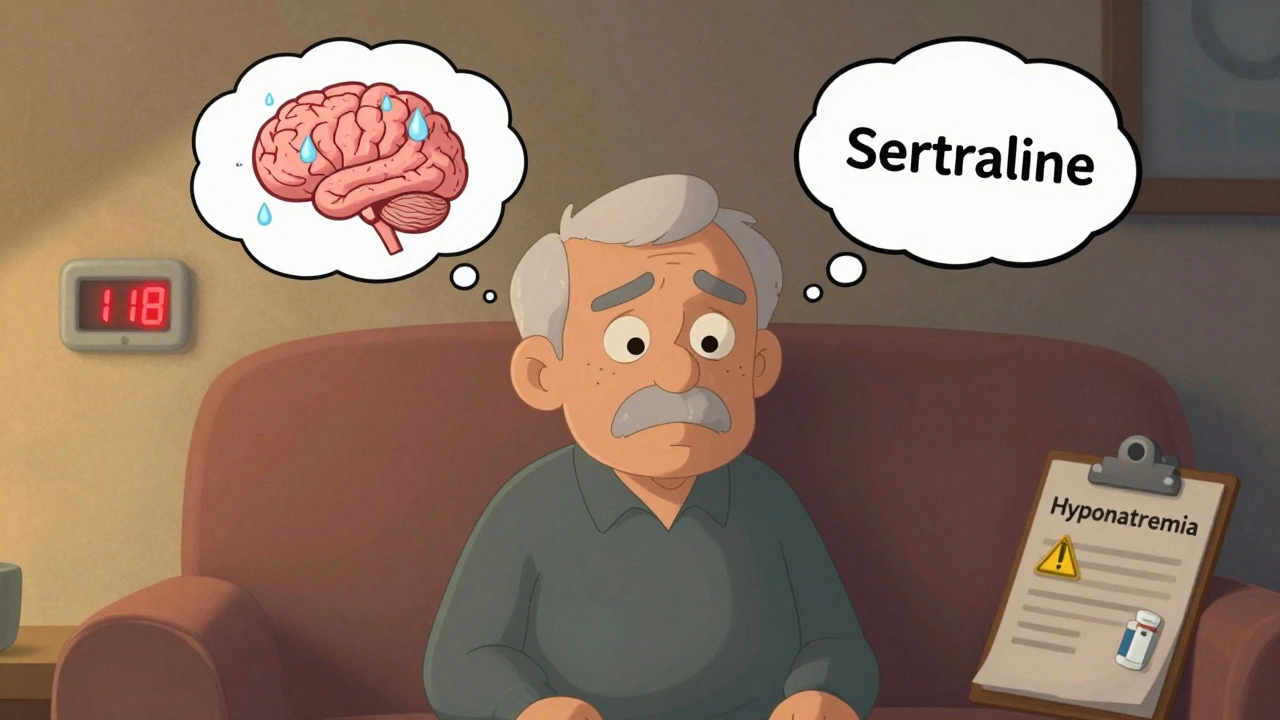
Hyponatremia means your blood sodium is below 135 mmol/L. Normal is 135-145. When it falls below 125, you’re in danger. At 118, as one 78-year-old woman experienced after starting sertraline, you end up in the ICU. Her symptoms? Confusion, nausea, stumbling. Doctors thought it was dementia. It wasn’t. It was the drug.
How SSRIs Cause Low Sodium
SSRIs work by boosting serotonin in the brain. That’s good for mood. But serotonin also acts on the hypothalamus-the part of your brain that controls how much water your kidneys hold onto. Too much serotonin = too much antidiuretic hormone (ADH) = your body keeps water instead of flushing it out.
This isn’t dehydration. It’s water intoxication. Your blood gets diluted. Sodium drops. Your brain swells slightly. That’s why you get headaches, confusion, or trouble walking. It’s not mental decline. It’s chemical.
Not all SSRIs are equal. Citalopram has the highest risk-over twice as likely as some others. Sertraline and fluoxetine follow close behind. Paroxetine is lower, but still risky. Why? It’s about how tightly they bind to the serotonin transporter. The tighter the grip, the more ADH gets released.
Who’s Most at Risk
This isn’t a problem for everyone. But for some, the risk is sky-high:
- Age 65+: Your kidneys don’t handle water the same way. Risk jumps to 14-19%.
- Women: Over 65% of cases occur in women, likely due to body size and hormonal differences.
- Low body weight: Under 60 kg? Your blood volume is smaller. Less water to dilute.
- On diuretics: Thiazide diuretics (like hydrochlorothiazide) make this risk 4 times worse. Many older adults take them for high blood pressure.
- Renal impairment: If your eGFR is under 60, your kidneys can’t clear water efficiently.
- Starting or increasing dose: The biggest spike in risk happens in the first 2-4 weeks.
One man in his 80s took citalopram for depression. Two weeks later, he stopped recognizing his grandchildren. His sodium? 122 mmol/L. He was hospitalized. The doctor didn’t connect the dots until the family mentioned the new pill.
What Symptoms to Watch For
Early signs are easy to miss. They look like aging, stress, or just "getting older." But they’re not.
- Headaches that won’t go away
- Nausea or loss of appetite
- Feeling unusually tired or weak
- Mild confusion or trouble remembering things
- Walking unsteadily or feeling off-balance
- Muscle cramps or twitching
By the time someone is having seizures or slipping into a coma, it’s too late. The warning signs are subtle. If you or a loved one starts an SSRI and begins acting "not themselves," check sodium levels. Don’t wait.
How Doctors Should Be Testing
It’s not complicated. But too many doctors skip it.
The American Psychiatric Association says: Test sodium before starting an SSRI, then again at 2 weeks. For high-risk patients, test monthly for the first 3 months.
Here’s what they’re looking for:
- Serum sodium < 135 mmol/L
- Urine sodium > 30 mmol/L (your kidneys are holding onto salt)
- Urine osmolality > 100 mOsm/kg (your body is concentrating urine too much)
- No signs of dehydration or heart failure (it’s euvolemic SIADH)
A 2023 survey found that 63% of primary care doctors didn’t know the typical onset window was 2-4 weeks. That’s why cases get missed. It’s not the patient’s fault. It’s a system gap.
What to Do If Sodium Drops
What happens next depends on how low it goes.
Mild hyponatremia (125-134 mmol/L):
- Stop the SSRI immediately
- Limit fluids to 800-1000 mL per day
- Recheck sodium in 48 hours
- Recovery usually happens in 3-4 days
Severe hyponatremia (<125 mmol/L):
- Hospitalization required
- IV hypertonic saline (3%) given slowly-no more than 6-8 mmol/L increase in 24 hours
- Too fast correction can cause brain damage (osmotic demyelination)
- Recovery takes days to weeks
One woman in Oxford had her sodium drop to 118 after starting sertraline. She was confused, couldn’t stand without help. They stopped the drug and gave her saline. It took 5 days for her to return to normal. She didn’t go back on any SSRI.
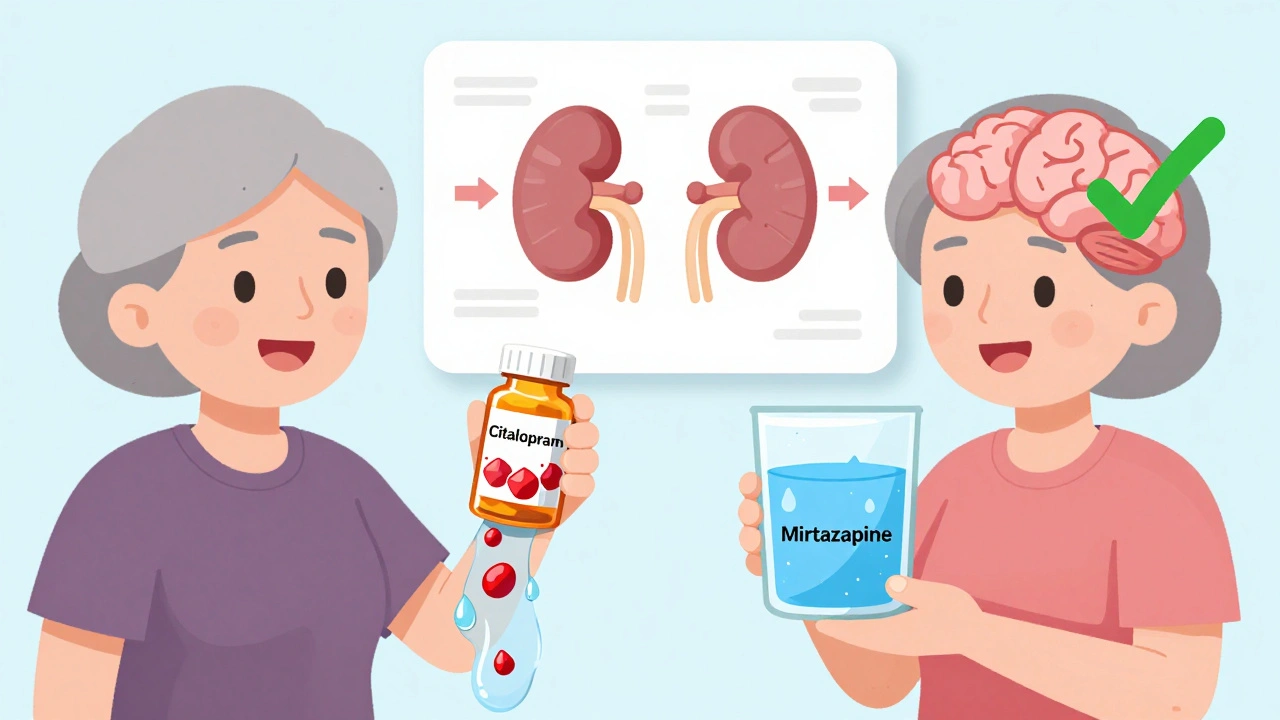
Better Alternatives for Older Adults
There are antidepressants that don’t carry this risk.
Mirtazapine is the clear winner. Studies show it has less than half the risk of SSRIs. In fact, for every 1,000 older adults treated with mirtazapine, only 6-7 develop hyponatremia. With SSRIs? 18-20. That’s a number needed to harm (NNH) of 82. Meaning, if you switch 82 elderly patients from an SSRI to mirtazapine, you prevent one case of dangerous low sodium.
Bupropion is another good option. It doesn’t affect serotonin the same way. Risk is low-about the same as placebo. It’s not ideal for everyone (can cause insomnia or anxiety), but it’s safe for sodium.
SNRIs like venlafaxine and duloxetine? Still riskier than mirtazapine. Tricyclics like amitriptyline? Also risky. Stick to mirtazapine or bupropion for older patients.
The American Geriatrics Society’s 2023 Beers Criteria lists SSRIs as potentially inappropriate for seniors because of hyponatremia. Mirtazapine is recommended instead.

Why This Is Still Underdiagnosed
Most cases go unnoticed.
A 2023 survey found only 29% of patients were told about this risk before starting SSRIs. Doctors assume confusion means dementia. Families think it’s just aging. Emergency rooms see "unexplained falls" and don’t test sodium.
One study found 38% of mild cases in primary care are never caught. That means hundreds of thousands of older people are walking around with low sodium-increasing their risk of falls, fractures, and long-term cognitive decline.
It’s not just a side effect. It’s a silent crisis.
What You Can Do
If you or someone you care for is on an SSRI and over 65:
- Ask for a baseline sodium test before starting the drug.
- Ask for a repeat test at 2 weeks.
- Watch for any change in thinking, balance, or appetite.
- If symptoms appear, get sodium checked immediately-don’t wait.
- Ask if mirtazapine or bupropion could be a safer alternative.
Don’t assume the doctor knows. Ask. Push. Keep a symptom diary. This isn’t paranoia. It’s prevention.
Antidepressants save lives. But they shouldn’t trade one risk for another. With the right monitoring and alternatives, you can treat depression without putting someone’s brain at risk.
What’s Changing in 2025
The FDA now requires SSRI labels to warn about hyponatremia. The European Medicines Agency is reviewing safety data-results expected by fall 2025. In the U.S., prescriptions for SSRIs in patients over 65 dropped 22% between 2018 and 2023. Mirtazapine prescriptions for that group rose 35%.
By 2027, mirtazapine could be the top choice for older adults needing antidepressants. That’s progress. But it’s not fast enough.
Every year, $1.27 billion is spent in the U.S. treating SSRI-induced hyponatremia-mostly in hospitals and ERs. Most of it could have been avoided with a simple blood test.
Can SSRIs cause confusion in older adults?
Yes. SSRIs can cause hyponatremia-low sodium in the blood-which leads to confusion, disorientation, memory problems, and even seizures in severe cases. These symptoms are often mistaken for dementia or normal aging, especially in older adults. If confusion starts within 2-4 weeks of beginning an SSRI, low sodium should be ruled out with a blood test.
Which SSRI has the highest risk of causing low sodium?
Citalopram carries the highest risk among SSRIs, with over twice the likelihood of causing hyponatremia compared to some others. Sertraline and fluoxetine also have significantly elevated risk. Paroxetine is lower but still risky. The risk is tied to how strongly the drug binds to the serotonin transporter-tighter binding means more water retention.
Is mirtazapine safer than SSRIs for seniors?
Yes. Mirtazapine has the lowest risk of hyponatremia among antidepressants-less than half the risk of SSRIs. It’s recommended by the American Geriatrics Society as a safer first-line option for older adults. Studies show only 6-7 cases per 1,000 patients on mirtazapine versus 18-20 per 1,000 on SSRIs. For seniors, it’s often the better choice.
How soon after starting an SSRI can hyponatremia develop?
Hyponatremia typically appears within 2 to 4 weeks after starting an SSRI or increasing the dose. It’s rare before 1 week and uncommon after 6 weeks. That’s why doctors recommend checking sodium levels at the 2-week mark-timing matters for early detection.
Should I stop my SSRI if I feel confused?
Don’t stop abruptly without medical advice. But if you feel confused, unsteady, or nauseous after starting an SSRI, get a blood test for sodium immediately. If hyponatremia is confirmed, your doctor will likely stop the SSRI and may replace it with a safer alternative like mirtazapine. Never ignore new neurological symptoms after starting a new medication.
Can I still take an SSRI if I’m over 65?
Yes-but only with precautions. If you’re over 65, ask for a sodium test before starting and again at 2 weeks. Avoid SSRIs if you’re on diuretics, have kidney issues, or are underweight. Ask your doctor if mirtazapine or bupropion could work instead. With monitoring, SSRIs can be used safely, but they’re not the safest option for older adults.
Final Thought
Depression in older adults is real. So is the risk of these drugs. You don’t have to choose between feeling better and staying safe. With the right test, the right drug, and the right questions, you can avoid the silent danger of low sodium. Ask for the blood test. Ask about alternatives. Your brain is worth it.
8 Comments
Jane Quitain
I had no idea SSRIs could do this. My mom started sertraline last month and kept stumbling around like she was drunk. We thought it was just old age... turns out her sodium was 121. They pulled the pill and she bounced back in 3 days. Why isn't this on every prescription label?
Ted Rosenwasser
The pathophysiology here is textbook SIADH, but the real issue is the complete lack of clinical vigilance in primary care. SSRIs are prescribed like candy, and serum sodium isn't even on the differential for 'confusion in elderly.' The APA guidelines are clear, but implementation is abysmal. This isn't a drug problem-it's a systems failure rooted in cognitive bias and time poverty.
Oliver Damon
It’s fascinating how a molecule designed to modulate mood ends up hijacking renal water homeostasis. Serotonin’s dual role in the CNS and renal tubules is a perfect example of pleiotropy gone wrong. The binding affinity to SERT correlates directly with ADH release, which explains why citalopram is the worst offender. But here’s the kicker-most clinicians don’t even know what SIADH stands for. We’re treating symptoms while ignoring the mechanism. That’s not medicine. That’s triage with a placebo mindset.
Kurt Russell
THIS IS A PUBLIC HEALTH CRISIS AND NO ONE IS TALKING ABOUT IT. My uncle was misdiagnosed with Alzheimer’s because his sodium dropped to 118. He was 79. They put him in a memory unit for MONTHS. He was just dehydrated from his own body holding water because of citalopram. When they finally checked his labs? He cried. He said, 'I just wanted to feel better.' Stop prescribing these like they’re vitamin supplements. Test sodium. Before. And at 2 weeks. That’s it. That’s the fix.
Louis Llaine
So let me get this straight. We’re telling old people to stop taking antidepressants because they might get confused... but we’re fine with them taking 7 other pills that cause falls, kidney damage, and dementia? This is just fearmongering dressed up as medical advice. Next you’ll say caffeine causes hyponatremia.
Sam Mathew Cheriyan
lol i think this is all part of the pharmabig coverup. they dont want you to know that water is actually the real cause of depression. if you drink less water, your sodium goes up and you feel happy. SSRIs are just a distraction so they can sell more pills. my cousin in india stopped his meds and drank 2 liters of salt water. now he’s dancing at weddings. true story.
Ernie Blevins
So you're saying we should stop giving people hope just because their sodium might dip? What's next? Ban antidepressants because someone might get a headache? This isn't science. This is guilt-tripping vulnerable people who are already broken. You're not helping. You're just making them feel worse.
David Brooks
This is the kind of post that changes lives. I shared it with my entire family. My grandma is on sertraline and we’re getting her sodium checked tomorrow. If this saves even one person from being misdiagnosed as demented, it’s worth it. Thank you for writing this. People like you are the reason I still believe in medicine.






Write a comment