Commercial Driving and Medications: What You Must Know for Safety and Compliance
Commercial Driving Medication Checker
Check Your Medications
Enter medications you take to see if they're compliant with FMCSA regulations.
What Medications Can Keep You Off the Road?
If you drive a commercial truck or bus, the pills you take every day could cost you your job-even if they’re prescribed by a doctor. The Federal Motor Carrier Safety Administration (FMCSA) doesn’t care if your medication helps you sleep, manage pain, or focus. If it could make you drowsy, dizzy, or slow to react, it’s banned. And the rules aren’t suggestions. They’re enforced with roadside inspections, drug tests, and digital tracking systems that flag violations in real time.
In 2020, over 1,200 people died in crashes involving commercial drivers who tested positive for disqualifying substances. That’s not just a statistic. It’s why the FMCSA spends nearly $200 million a year on compliance checks and why your next DOT physical could be the most important medical appointment of your career.
The Hard Rules: What’s Actually Banned
The FMCSA doesn’t list every single drug. Instead, it bans entire categories based on how they affect driving ability. Schedule I drugs like marijuana, PCP, and heroin are automatic disqualifiers-even if you have a medical card in your state. But the real trap for most drivers is prescription and over-the-counter meds that seem harmless.
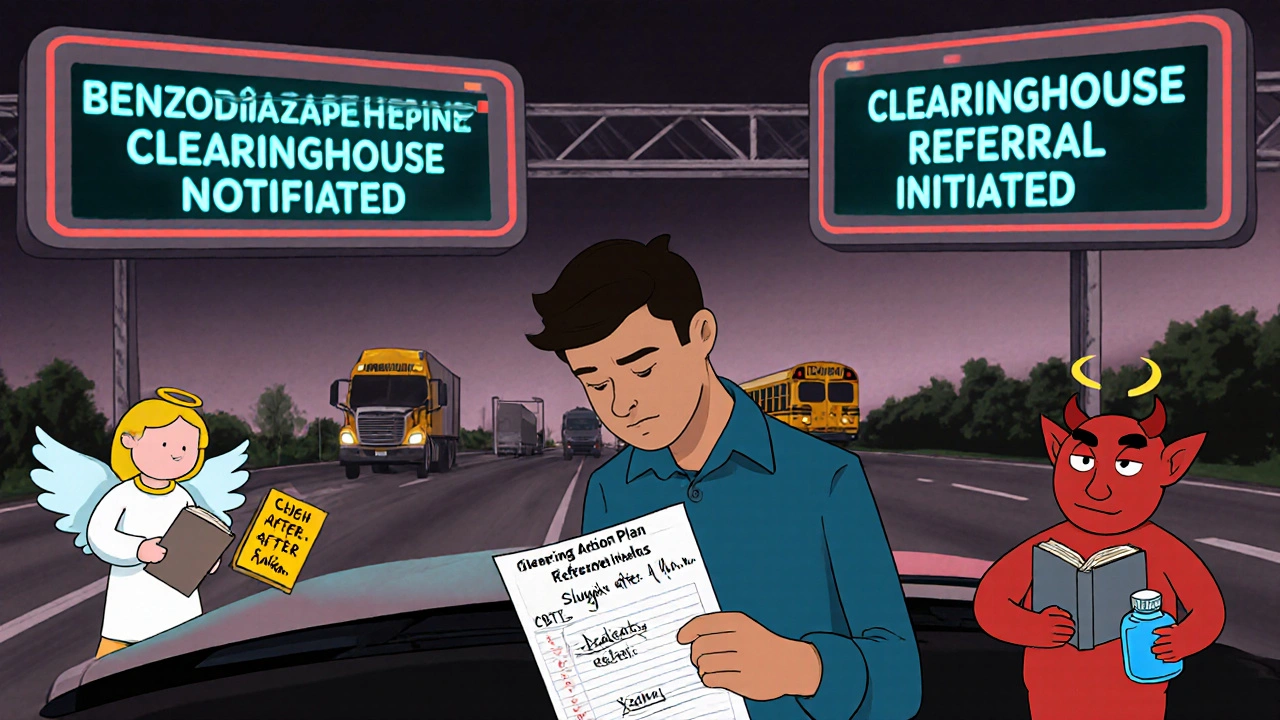
Amphetamines? Banned. That includes Adderall and Vyvanse, even if you’ve been taking them for ADHD since college. Narcotics like codeine, oxycodone, and hydrocodone? Also banned. Even if your doctor says you need them for chronic back pain, the FMCSA says no. Benzodiazepines like Xanax and Valium? Still prohibited, and starting in 2024, even prescription use must be reported to the Drug and Alcohol Clearinghouse within 24 hours.
And it’s not just pills. Over-the-counter cold medicines with pseudoephedrine or dextromethorphan can trigger false positives on DOT drug screens. One driver in Ohio lost his CDL after taking a day’s dose of Robitussin DM. He didn’t know it was on the FMCSA’s list of potential impairers.
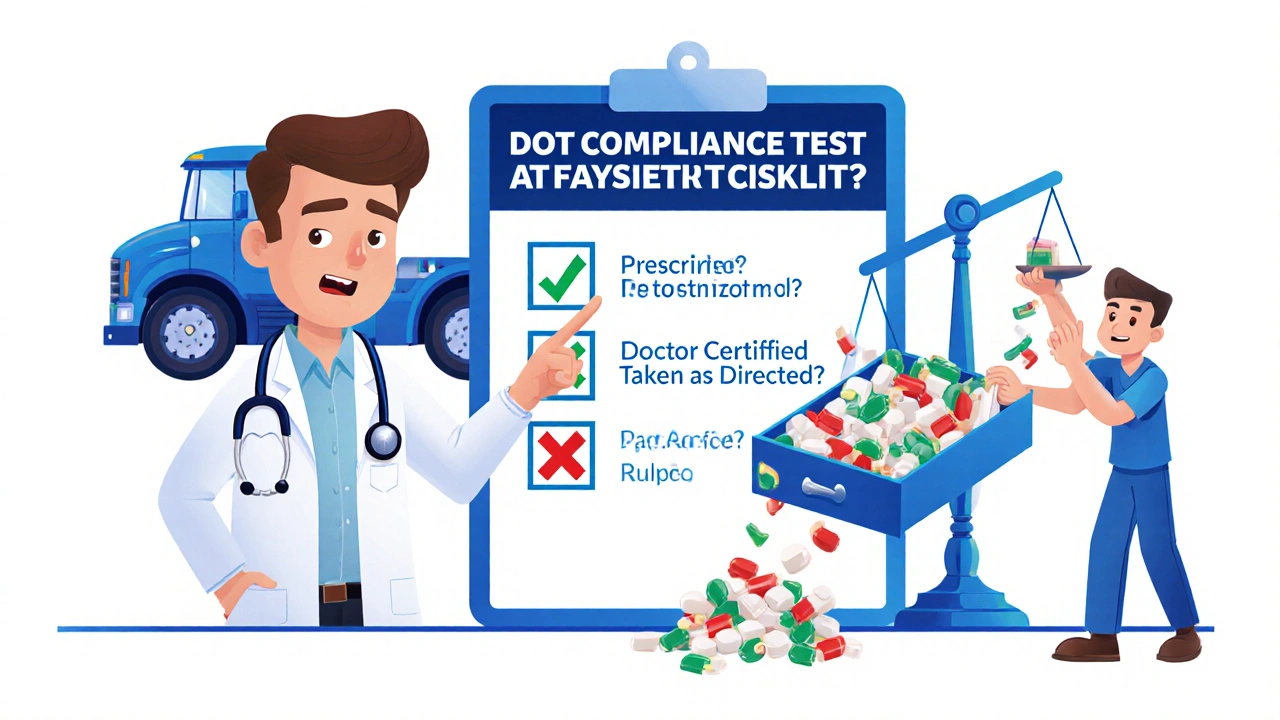
What’s Allowed? The Three-Part Test
Not all medications are off-limits. The FMCSA allows some if they meet three strict conditions:
- The drug must be prescribed by a licensed physician.
- The doctor must certify in writing that the medication won’t interfere with safe driving.
- You must take it exactly as prescribed-no extra doses, no skipping doses, no mixing with alcohol.
That’s it. No exceptions. A driver with high blood pressure on lisinopril? Fine. A driver on gabapentin for nerve pain? Probably not. Even if your doctor says it’s safe, the Medical Examiner at your DOT physical has the final say. And they’re trained to say no more often than you think.
According to Dr. Gary Solomon, a certified Medical Examiner with over 20 years of experience, 35% of drivers he examines are on medications that require special review. Antidepressants are the most common. But even SSRIs like sertraline or fluoxetine can be flagged if the driver has side effects like drowsiness, blurred vision, or slowed reaction time.
Why the Rules Are So Strict (And Why They’re Not Changing Soon)
Compare the U.S. to Europe. In Germany, France, and the Netherlands, commercial drivers can legally use certain narcotics if they’re under doctor supervision and show no signs of impairment. In the U.S.? Zero tolerance. Why? Because the stakes are higher. A passenger bus full of kids, a tanker carrying hazardous materials, an 80,000-pound truck on a rainy interstate-these aren’t cars. One second of delayed reaction can mean dozens of deaths.
There’s also a legal reality: if you’re in a crash and you’re on a banned medication-even if it’s legal for you-the company, the driver, and the medical examiner can all be sued. Insurance companies won’t pay. Courts don’t care if you were “just following your doctor’s orders.” The FMCSA rule is the law. End of story.
And despite pressure from driver groups, the rules aren’t getting looser. In fact, they’re tightening. The 2024 proposal to include all benzodiazepines in mandatory reporting came after NHTSA found a 22% spike in positive crash tests since 2019. The FMCSA isn’t trying to punish drivers. They’re trying to prevent bodies from piling up on the highway.
What Happens When You Get Caught?
If you test positive for a disqualifying drug, you’re immediately removed from safety-sensitive duties. That means no driving, no dispatch, no paycheck. You’ll be referred to a Substance Abuse Professional (SAP) for evaluation. The SAP will determine if you need counseling, rehab, or both. Only after completing the program and passing a return-to-duty test can you even apply to get your CDL back.
But it’s not just you. Your employer gets fined. The average penalty for failing to manage driver medication compliance is $14,200. And if your company doesn’t report your violation to the Drug and Alcohol Clearinghouse within 24 hours? Another $1,250 fine-per incident.
And here’s the kicker: your violation stays on the Clearinghouse for five years. Future employers can see it. Even if you’re cleared to drive again, your record follows you. One driver in Texas told TruckersReport.com he applied for 37 jobs after completing his SAP program. Only two called him back.
What Can You Do If You Need a Banned Medication?
If you’re on a banned drug and you need it to function, you have options-but they’re not easy.
First, talk to your doctor. Not just any doctor. A doctor who understands commercial driving rules. Tell them your job. Show them your CDL. Ask: “Is there an alternative that’s DOT-compliant?”
For ADHD: Strattera (atomoxetine) is a non-stimulant that’s allowed. For chronic pain: non-opioid options like duloxetine or physical therapy might work. For sleep: CBT-I (cognitive behavioral therapy for insomnia) is more effective than sleep aids and fully compliant.
Second, if you absolutely can’t switch, apply for a Skill Performance Evaluation (SPE) certificate. It’s not a waiver. It’s a performance test. You’ll drive under observation, with your doctor’s documentation, to prove you can operate safely. The approval rate is 68%. But it takes 6-12 weeks. And it costs money.
Third, document everything. Keep a Medication Action Plan. Note how each drug affects you: “After taking my antidepressant, I feel sluggish after 2 p.m. I avoid driving after 4 p.m.” That’s not just advice-it’s required by the FMCSA’s own guidelines.
The Real Cost of Compliance
Getting your DOT physical costs $85-$150. The Medication Action Plan? Free if you make it yourself. But the hidden costs are higher.
Over 60% of drivers surveyed by OOIDA said they stopped taking effective medications because of DOT rules. 41% said their health got worse. Some switched to illegal drugs. Others drove while in pain. One driver in Iowa told investigators he stopped taking his blood pressure meds because he couldn’t afford the copay and didn’t want to risk losing his job. He had a stroke at a rest stop.
And for companies? The cost of compliance has jumped 42% since 2020. Most carriers now use electronic systems to track driver meds. But 28% still fail audits. Why? Because they assume “if it’s prescribed, it’s okay.” It’s not.
What’s Next for Commercial Drivers?
The FMCSA is testing wearable tech that monitors heart rate, eye movement, and steering patterns to detect impairment in real time. Pilot programs with Samsara and KeepTruckin are already underway. If they work, drivers might be able to prove they’re safe-even if they’re on a medication that’s normally banned.
But that’s years away. For now, the rules haven’t changed. And they won’t until the death toll drops.
If you’re a driver, your job depends on honesty. Not just with your employer. With your doctor. With yourself. Because the road doesn’t care if you’re in pain. It only cares if you’re alert.
How to Stay Compliant: A Quick Checklist
- Know your meds: Keep a printed list of every prescription, OTC, and supplement you take.
- Disclose everything at your DOT physical-even vitamins and herbal teas.
- Ask your doctor: “Is this safe for a commercial driver?” Don’t assume.
- Never drive if you feel drowsy, dizzy, or unfocused-even if you think it’s “just a little.”
- Update your Medication Action Plan every time your dosage changes.
- Report any medication changes to your employer within 24 hours.
- Know the FMCSA’s list of prohibited substances. Bookmark it. Read it every six months.
What Happens If You Don’t Follow the Rules?
You don’t just risk your license. You risk your life-and other people’s.
One driver in Georgia lost his CDL after taking tramadol for a herniated disc. He fell asleep at the wheel and rear-ended a semi carrying gasoline. Two people died. He served 18 months in prison. His company went bankrupt from lawsuits.
That’s not a horror story. It’s a common outcome.
The FMCSA doesn’t want to take your job. They want to keep you alive. But they can’t protect you if you won’t protect yourself.
12 Comments
Sue Barnes
This is why I stopped taking my Xanax. Not because I didn't need it, but because I didn't want to risk losing my CDL over a pill that makes me feel like a zombie anyway. The FMCSA isn't being cruel-they're being the only thing standing between a truck and a school bus full of kids. No sympathy for people who think 'it's just a little drowsy'-that's how you end up in the obituary.
jobin joshua
Bro, I took Robitussin DM for a cold last winter and got flagged 😭. My boss said 'sorry bro, but your meds are worse than weed'. I cried in the parking lot. 🥲
Sachin Agnihotri
I get it, safety is huge-but have you ever tried living on $12/hour without pain meds? My back is shot from hauling steel for 15 years. I'm not asking for a free pass, just a little mercy. The system feels like it's punishing the people it claims to protect. 🤔
Diana Askew
They're lying. The real reason they ban everything? Big Pharma doesn't want you to take cheap OTC stuff-they want you on their $500/month 'approved' meds. The DOT's just their puppet. And don't get me started on the Clearinghouse-it's a black box that destroys lives. I know a guy who got banned for melatonin. 😡
King Property
You people act like this is a hardship. Let me break it down for you: If you're so weak you need Adderall to focus, you shouldn't be driving 80,000 pounds at 70 mph. If you need opioids for pain, you're not fit to operate heavy machinery. Period. The fact that you're even debating this shows how broken the system is-and how many drivers are just one bad decision away from killing someone. Stop whining. Get healthy or get out.
Yash Hemrajani
Ah yes, the classic 'I need my meds' cry. Let me guess-you're also the guy who thinks 'natural remedies' are better than science? Lol. Strattera for ADHD? CBT-I for sleep? Dude, you're not a pioneer-you're just late to the memo. The rules are clear. Adapt or get left behind. And no, 'I'm in pain' doesn't override physics. Your spine doesn't get a pass when you're behind the wheel.
Pawittar Singh
Hey, I’ve been there. Took gabapentin for nerve pain, got flagged. Thought my career was over. But I found a DOT-savvy doc, switched to duloxetine, started physical therapy, and now I’m back on the road. It’s not easy-but it’s possible. You’re not broken. You just need to play the game right. 💪 You got this. And if you need help finding a good SAP, DM me. I’ve been through it.
Josh Evans
I used to think the rules were too strict. Then I saw a crash video where a guy on hydrocodone T-boned a family minivan. Two kids dead. He was just trying to sleep. I cried. Now I check every med I take against the FMCSA list. It’s not about trust-it’s about responsibility.
Allison Reed
The checklist at the end? Perfect. Print it. Laminate it. Tape it to your dashboard. Knowledge is power-but only if you use it. And if you're struggling with side effects, talk to your doctor. Not your buddy at the truck stop. Your doctor. They can help you find alternatives that keep you safe and on the road.
Jacob Keil
I mean, like, if the government wants to control what we take, then why not just give us all brain implants? That'd be more efficient than this bureaucratic nightmare. They say 'zero tolerance' but they don't say 'zero empathy'. We're not criminals-we're workers trying to survive. And honestly? The real danger isn't the meds-it's the system that makes us choose between health and a paycheck.
Rosy Wilkens
The FMCSA is a front for the corporate elite. They don't care about safety-they care about liability. That’s why they ban everything. They know if they allow even one exception, lawsuits will flood in. So they make it impossible. And then they charge you $150 for a physical that’s just a formality. This isn’t safety. It’s exploitation dressed up as regulation.
Andrea Jones
Okay, so you’re on gabapentin and your doc says it’s fine-but the ME says no? That’s frustrating. But here’s the thing: you’re not alone. I’ve seen drivers go from depressed to thriving after switching to CBT-I. It’s not glamorous, but it works. And hey-if you’re scared to ask your doctor, just say, 'I need to keep my CDL. What’s the safest option?' They’ll get it. You’re not weak for needing help. You’re smart for asking.






Write a comment