FDA Biosimilars: What They Are, How They Work, and Why They Matter
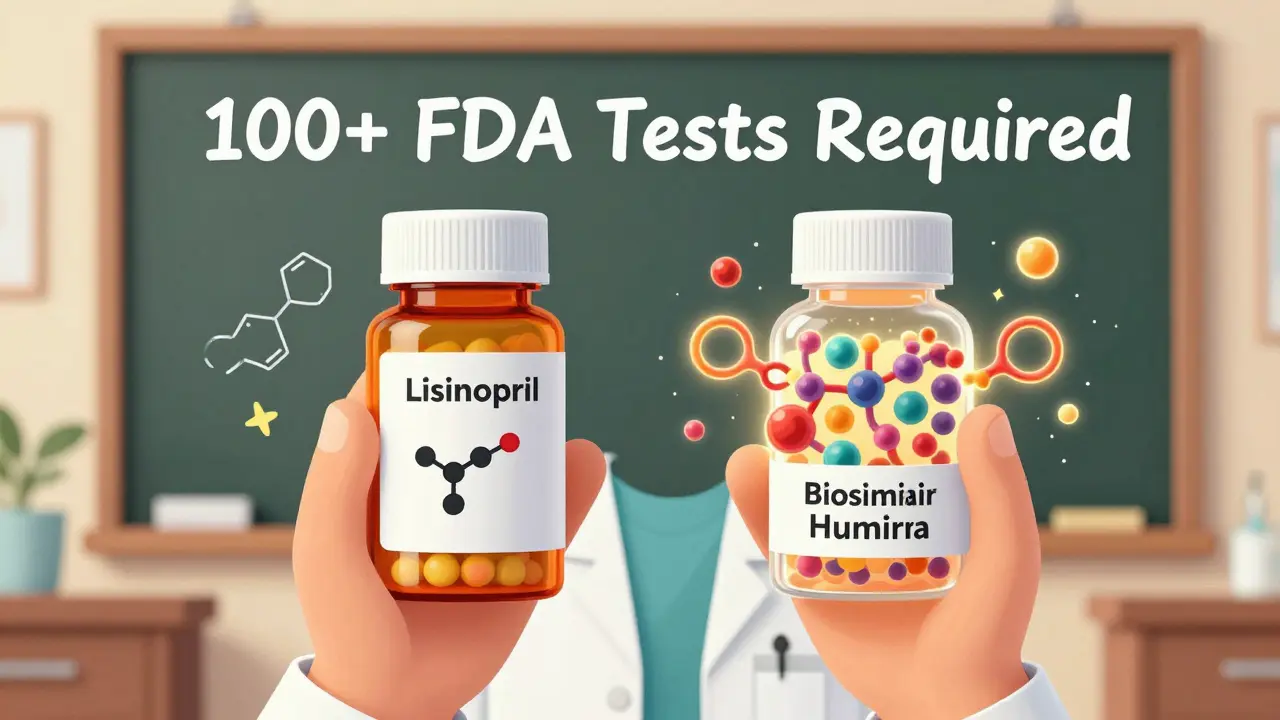
When you hear FDA biosimilars, approved versions of complex biologic medications that match the original in safety, purity, and potency. Also known as biologic generics, they are not simple copies like traditional pills—they’re made from living cells and require rigorous testing to prove they work just like the original. Unlike regular generics, which are chemically identical to their brand-name counterparts, biosimilars are highly similar but not exact matches because biologics are too complex to replicate perfectly. The FDA doesn’t just approve them based on price—it demands proof they deliver the same clinical results, with no meaningful difference in safety or effectiveness.
These drugs are changing how we treat conditions like rheumatoid arthritis, cancer, and diabetes. For example, biologics, large, protein-based drugs made from living organisms, often used for autoimmune and chronic diseases like Humira or Enbrel used to cost over $2,000 a month. Now, biosimilars like Cyltezo or Amjevita cut that cost by 30% to 50%, without compromising outcomes. The FDA requires bridging studies, clinical trials that compare biosimilars directly to the original biologic to confirm they behave the same in the body—the same kind of rigorous testing you’ll see in posts about NTI generics, but even more complex because biologics are sensitive to tiny changes in manufacturing.
It’s not just about savings. Biosimilars increase access. Many patients couldn’t afford the original biologic, so they went without treatment. Now, with biosimilars, more people get the drugs they need. But confusion still exists. Some think biosimilars are inferior, or that switching from a brand-name biologic to a biosimilar is risky. The FDA says otherwise. Multiple studies, including real-world data from Medicare and VA systems, show patients do just as well—or better—on biosimilars. And the agency keeps a public database so doctors and patients can track which biosimilars are approved and for what conditions.
You’ll also find that biosimilars don’t replace all biologics overnight. Drugmakers sometimes delay them with legal tricks, like changing the original drug’s packaging or delivery method just before the patent expires—a tactic called product hopping. That’s why posts about antitrust issues in generic substitution matter here too. The same forces that block cheap pills can try to block cheaper biologics. The FDA fights back with clear guidelines, but patients and providers need to know their rights.
What you’ll find in this collection isn’t just theory. It’s real-world insight: how biosimilars are tested, how they compare to the originals, how pharmacies verify them, and how they fit into treatment plans for diabetes, arthritis, and cancer. You’ll see how pharmacogenomics and dosing precision play a role, and why some patients need extra monitoring even after switching. No fluff. No marketing. Just what you need to understand your options—and make smarter choices with your doctor.
Provider Education: Understanding Biosimilar Differences
Biosimilars are not generics-they're complex, FDA-approved copies of biologic drugs that require special understanding. Learn how they differ, why providers hesitate, and what you need to know to use them safely and effectively.
Read MoreHow to Understand Biosimilars and Their Cost Implications
Biosimilars offer the same effectiveness as expensive biologic drugs at 15-30% lower cost. Learn how they work, why they’re safe, and how they’re changing access to life-saving treatments.
Read More