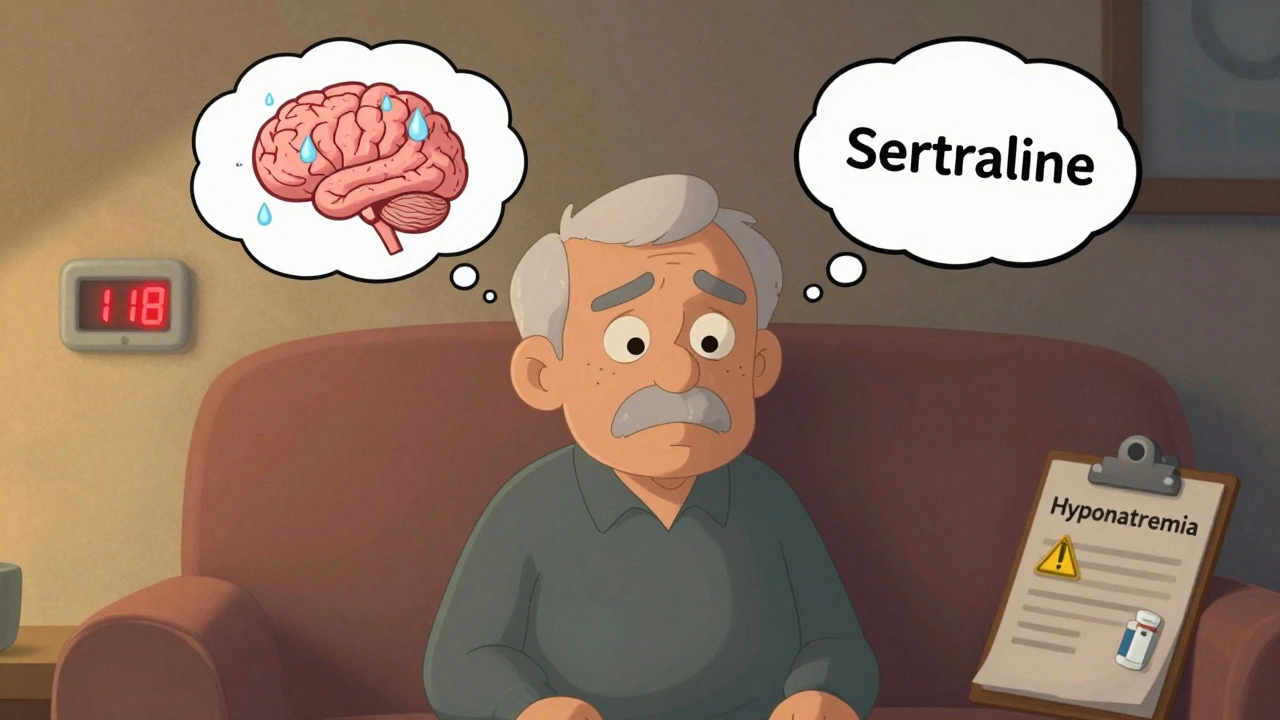
SSRI Hyponatremia: What You Need to Know About Low Sodium and Antidepressants
When you take an SSRI, a class of antidepressants that increase serotonin levels in the brain, commonly used to treat depression and anxiety. Also known as selective serotonin reuptake inhibitors, these drugs help millions feel better—but they can also cause a dangerous drop in blood sodium, called hyponatremia, a condition where sodium levels in the blood fall below 135 mmol/L, leading to confusion, seizures, or even coma. This isn’t rare. Studies show up to 1 in 10 older adults on SSRIs develop this side effect, especially within the first few weeks of starting the medication.
SSRIs like Lexapro, Zoloft, and Prozac trigger hyponatremia by messing with how your kidneys handle water. Normally, your body balances sodium and water tightly. But SSRIs overstimulate a hormone called ADH, which tells your kidneys to hold onto water instead of flushing it out. That dilutes your sodium. It’s not about drinking too much water—it’s about your body holding onto too much of it. People over 65, women, and those on high doses or multiple medications are most at risk. If you’re on an SSRI and start feeling unusually tired, nauseous, or confused, don’t assume it’s just your depression coming back. Check your sodium levels.
This problem connects directly to other medication safety topics you’ll find here. For example, just like warfarin needs careful monitoring because small changes can throw off your INR, SSRIs need the same attention when it comes to sodium. The same caution applies to lithium, a mood stabilizer that also affects kidney function and is easily pushed to toxic levels by other drugs. Lithium and SSRIs together? That’s a double hit on your kidneys and electrolytes. And if you’re taking NSAIDs like ibuprofen for pain, you’re adding another layer of risk. These aren’t just theoretical concerns—they’re real, documented dangers that show up in clinics and emergency rooms.
What makes this even trickier is that hyponatremia often flies under the radar. You might feel fine until you suddenly stumble, vomit, or lose focus. Many doctors don’t test sodium unless symptoms are obvious. But if you’re on an SSRI and you’re older, female, or taking other meds that affect your kidneys, ask for a simple blood test early on. It’s not a big deal—it’s a smart move. And if your sodium drops, it doesn’t mean you have to stop your antidepressant. Often, lowering the dose, switching to a different SSRI, or adjusting fluid intake fixes it. The goal isn’t to avoid treatment—it’s to manage it safely.
Below, you’ll find real-world posts that dig into the same kind of medication risks: how generic switching affects blood thinners, how herbal supplements interfere with diabetes drugs, and why even common painkillers can turn dangerous when mixed with psychiatric meds. These aren’t abstract warnings. They’re stories from people who’ve been there—and from pharmacists who’ve seen the fallout. If you’re on an SSRI, or caring for someone who is, this collection gives you the facts you need to stay safe without fear.
Hyponatremia from SSRIs: Low Sodium and Confusion Risk in Older Adults
SSRIs can cause dangerously low sodium levels, especially in older adults, leading to confusion and falls. Learn who’s at risk, which antidepressants are safer, and what tests to ask for.
Read More