Urine Leakage and Sexual Health: What You Need to Know

Incontinence Type Identifier
This tool helps you identify whether your urine leakage is likely due to stress incontinence or urge incontinence based on your symptoms. Select the options that best describe your experience.
When Urinary Incontinence (commonly called urine leakage) hits, it can feel like an embarrassing bolt out of the blue, many people wonder how it will mess with their love life. The reality of urine leakage is that it often shows up at the worst moments, but understanding why it happens and what you can do about it puts the power back in your hands.
What Causes Urine Leakage?
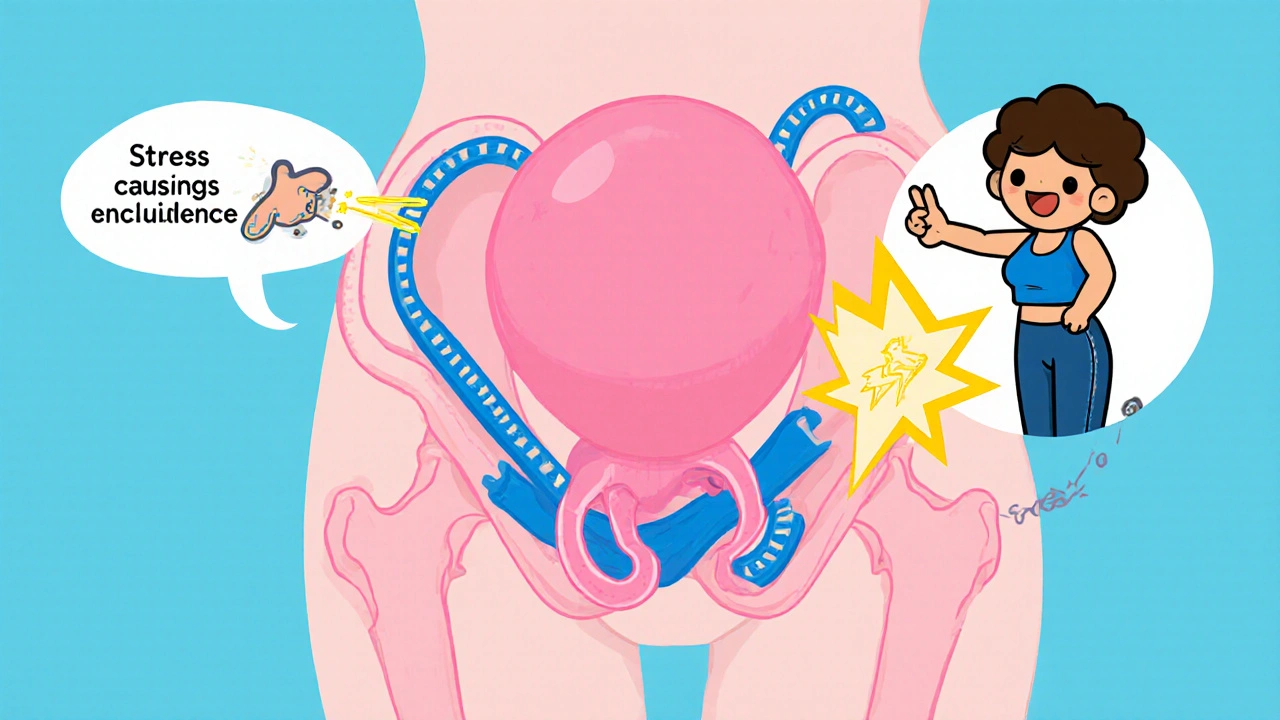
First, it helps to know what’s actually happening inside the body. Your bladder is a rubber balloon that stores urine until you’re ready to go. A network of Pelvic Floor Muscles the group of muscles that support the bladder, uterus, and rectum acts like a sling, keeping the urethra closed until you purposely relax them.
When those muscles weaken, or the nerves that tell them when to tighten go haywire, urine can slip through. Two common patterns show up:
- Stress Incontinence leakage that occurs when pressure on the abdomen spikes, such as during coughing, sneezing, or lifting heavy objects.
- Urge Incontinence a sudden, intense urge to urinate followed by involuntary loss, often linked to an over‑active bladder.
Hormonal shifts, especially during menopause, can thin the lining of the urethra and reduce bladder capacity, making leakage more likely. Chronic conditions like diabetes, multiple sclerosis, or an enlarged prostate also play a role by damaging nerves or obstructing urine flow.
How Urine Leakage Affects Sexual Health
Sexual well‑being isn’t just about the act itself; it’s tied to confidence, intimacy, and emotional safety. When urine leaks during intimacy, several issues can arise:
- Erectile Dysfunction trouble achieving or maintaining an erection, often worsened by anxiety about leakage.
- Vaginal Dryness a common menopausal symptom that reduces lubrication, making intercourse uncomfortable and heightening fear of leaks.
- Psychological Impact feelings of embarrassment, lowered self‑esteem, and avoidance of sexual activity.
All of these feed into a feedback loop: anxiety triggers more leakage, which fuels more anxiety. Breaking that cycle starts with open communication and practical steps.
Talking Openly With Your Partner
Nothing cures the problem faster than a candid conversation. Here’s a quick script you can adapt:
- Choose a quiet moment, not right before or after intimacy.
- Explain what’s happening in plain terms-"I’ve been dealing with some bladder issues that cause occasional leaks. It’s not a reflection of how I feel about you."
- Invite questions and reassure them that you’re working on solutions.
- Discuss practical tips-extra pads, timing bathroom breaks, or trying positions that reduce pressure on the bladder.
Most partners appreciate honesty; it removes the mystery and lets the two of you tackle the issue together.
Physical Strategies to Reduce Leakage
Strengthening the pelvic floor is the cornerstone of non‑surgical treatment. The classic approach is Kegel Exercises targeted contractions that tighten the pelvic floor muscles. Here’s a simple routine:
- Identify the right muscles by stopping urine mid‑stream (don’t make this a habit, just for identification).
- Contract for 5 seconds, then relax for 5 seconds. Aim for 10 reps, three times a day.
- Progress to longer holds (up to 10 seconds) as strength improves.
Consistency matters more than intensity. Apps and biofeedback devices can help you track progress.
Other lifestyle tweaks that help:
- Limit caffeine and alcohol, both of which irritate the bladder.
- Maintain a healthy weight; excess pressure on the abdomen worsens stress incontinence.
- Practice timed voiding-go to the bathroom every 2‑3 hours to train the bladder.
Medical Options When Exercises Aren’t Enough
If pelvic floor training doesn’t bring relief after a few months, it’s time to explore medical avenues. A Medical Consultation with a urologist or pelvic health physiotherapist can pinpoint the exact cause and tailor treatment.
Typical options include:
- Prescription medications that calm an over‑active bladder (e.g., antimuscarinics).
- Topical estrogen creams for post‑menopausal women to improve urethral tissue quality.
- Minimally invasive procedures like bladder Botox injections or sling surgery, usually reserved for moderate‑to‑severe cases.
Regardless of the route, the goal is the same: restore confidence and protect intimacy.
Quick Comparison of Incontinence Types and Sexual Impact
| Feature | Stress Incontinence | Urge Incontinence |
|---|---|---|
| Typical Trigger | Coughing, sneezing, lifting | Sudden strong urge |
| Common Sexual Concerns | Leakage during thrusting or certain positions | Leakage right before climax, anxiety about timing |
| First‑line Treatment | Kegel exercises, weight management | Timed voiding, bladder training, meds |
| Effect on Partner | Often minimal once pads or timing are used | Higher anxiety due to unpredictability |
Key Takeaways
- Urinary incontinence is common and treatable; don’t let it dictate your love life.
- Identify whether stress or urge incontinence is driving the leaks to choose the right strategy.
- Open communication with your partner reduces embarrassment and builds teamwork.
- Consistent Kegel exercises, lifestyle tweaks, and timed voiding often improve symptoms.
- When self‑help isn’t enough, a medical consultation can open doors to meds, devices, or surgery.
Frequently Asked Questions
Can urine leakage happen during intercourse?
Yes. Pressure on the abdomen during certain positions or vigorous activity can force the bladder to release a small amount of urine, especially with stress incontinence.
Do Kegel exercises help both men and women?
Absolutely. For women, they tighten the muscles that control the urethra and vagina. For men, they strengthen the pelvic floor that supports the prostate and bladder, reducing leakage and even improving erectile function.
Is it safe to use disposable pads during sex?
Most disposable pads are thin enough to stay in place, but if you’re concerned about comfort, a washable, breathable incontinence liner works just as well and can be washed after use.
When should I see a doctor about incontinence?
If leaks occur more than once a week, cause skin irritation, affect intimacy, or are accompanied by pain, blood, or a sudden change in urine volume, schedule an appointment promptly.
Can hormonal therapy improve leakage after menopause?
Topical estrogen can thicken the urethral lining and improve muscle tone, which often reduces stress incontinence in post‑menopausal women. Discuss risks and benefits with your clinician.
12 Comments
brandon lee
Kegel routine works – just keep at it
Jill Raney
One must first acknowledge that the medical establishment has long been reluctant to disclose the full spectrum of non‑pharmaceutical solutions to urinary incontinence.
The veil of secrecy is not merely bureaucratic but appears orchestrated to sustain a lucrative market for invasive procedures.
Consider, for instance, the under‑promotion of rigorous pelvic floor training in mainstream health narratives.
The literature quietly references Kegel regimens, yet the popular press seldom amplifies their efficacy.
Such omission suggests an intentional marginalization of low‑cost, patient‑empowered interventions.
Moreover, the hormonal discourse surrounding menopause is often weaponized to perpetuate dependency on synthetic estrogen creams.
The subtle insinuation that only pharmaceuticals can restore urethral integrity diverges attention from simple lifestyle modifications.
By reducing caffeine intake, managing weight, and adhering to timed voiding schedules, many individuals experience measurable improvement.
The physiological basis for these recommendations is well‑documented in peer‑reviewed journals, yet they remain footnotes in public health advisories.
A critical reader will note the pattern: comprehensive, cost‑effective strategies are systematically downplayed.
In parallel, the psycho‑social impact of incontinence is frequently trivialized, ignoring the profound erosion of intimate confidence.
When partners are encouraged to discuss the condition openly, the stigma dissipates, and treatment adherence rises.
Therefore, fostering transparent communication is not a peripheral nicety but a therapeutic cornerstone.
The conscientious patient must, consequently, demand full disclosure from clinicians and seek out reputable pelvic health specialists.
Only through such vigilant advocacy can we dismantle the covert agenda that profits from our discomfort 😊😊.
Miah O'Malley
The bodily betrayals we experience often mirror the existential anxieties of our inner selves.
Leaking during intimacy can be read as a tangible manifestation of the fear of vulnerability.
Yet the mind is capable of re‑framing that moment into an act of shared authenticity.
When partners engage in honest dialogue, the metaphysical barrier of shame collapses.
Thus the physical and philosophical realms converge in a mutual healing process.
Joshua Pisueña
I appreciate the depth of your analysis it reinforces the need for patient empowerment through education and consistent pelvic floor training
Jhoan Farrell
Your openness about these challenges is truly brave 😊 It’s important to remember that many have walked this path and found relief through simple steps like timed voiding and Kegels 👏 Keep the conversation going, you’re not alone
Ryan Spanier
Dear colleague, your philosophical framing adds a valuable dimension to the discussion. It is essential to recognize that emotional intimacy is intertwined with physiological health. By encouraging transparent communication, we facilitate both mental and bodily resilience. I commend your thoughtful approach and hope it inspires further collaborative dialogue.
Abhinav Moudgil
What a vibrant tapestry of solutions we have at our disposal! From the rhythmic cadence of Kegel exercises to the subtle alchemy of dietary adjustments, each choice paints a brighter picture of confidence. Imagine the symphony of a well‑trained pelvic floor echoing through intimate moments, turning anxiety into assurance. Let us celebrate these tools with the exuberance they deserve, for they are the brushes with which we repaint our intimate lives.
Bradley Allan
Ah, the flamboyant flourish of colorful language! Yet, let us not be seduced by poetic flair alone-action, dear reader, is the crucible of change!!!
Without disciplined practice, all the rhetoric in the world remains hollow echo!!!
Commit to the regimen, and watch the drama of doubt dissolve into quiet triumph!!!
Kyle Garrity
I’ve been where you are, and I can say that consistency truly matters.
Start small, track your progress, and celebrate each improvement. You’re not alone in this journey.
Ralph Barcelos de Azevedo
While your supportive tone is commendable, let us not romanticize complacency. The moral imperative is to confront the issue head‑on, not merely soothe feelings. Accountability must accompany encouragement, lest we drift into passive acceptance.
Peter Rupar
Man this whole leaky talk is just a big hype train lol can't believe ppl still fall for it. Get real and stop overreacting.
Nikita Shue
Hey, tone it down a bit – it’s a legit health thing and not just a meme. If you’ve got concerns, actually talk to a pro instead of spouting nonsense.






Write a comment