A Deep Dive into the Pharmacokinetics of Bisoprolol

Bisoprolol is one of the most commonly prescribed beta-blockers for high blood pressure and chronic heart failure, yet few patients or even some clinicians fully understand how it moves through the body. Unlike older beta-blockers that rely heavily on liver metabolism, bisoprolol follows a unique path that makes it more predictable, safer, and easier to dose. If you’ve been prescribed bisoprolol and want to know why it works the way it does - or why your doctor chose it over other options - understanding its pharmacokinetics is key.
How Bisoprolol Gets Into Your Bloodstream
Bisoprolol is taken orally, usually as a tablet once a day. After swallowing, it starts moving through your digestive tract. Unlike some beta-blockers that get broken down heavily in the gut or liver before entering circulation, bisoprolol is absorbed efficiently - about 90% of the dose makes it into your bloodstream. That’s unusually high for a drug in its class. Most beta-blockers like propranolol or metoprolol are absorbed at only 50-70% due to first-pass metabolism.
It doesn’t need food to be absorbed, so you can take it with or without meals. Studies show that food doesn’t change how much of the drug enters your blood, though it might slightly delay absorption by about 1-2 hours. That’s not enough to affect its overall effectiveness. For most people, taking it at the same time each day - whether with breakfast or before bed - is more important than what you eat with it.
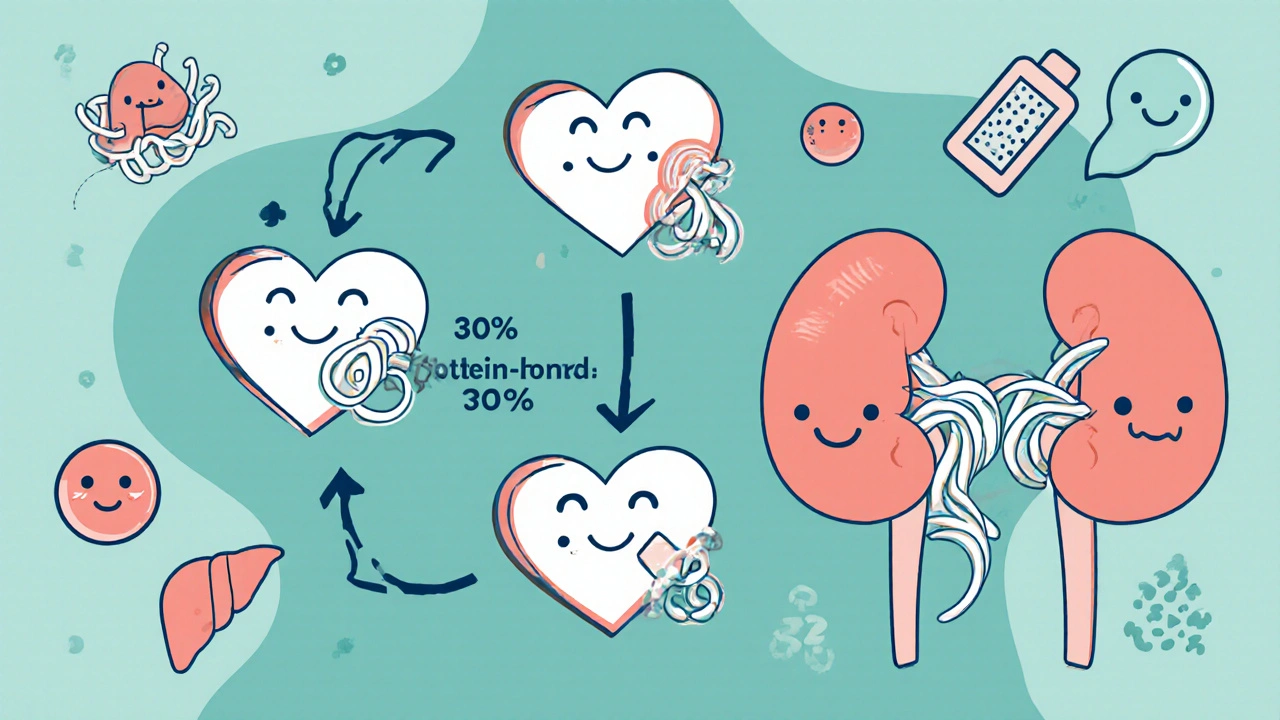
Where Bisoprolol Goes After Absorption
Once in the blood, bisoprolol doesn’t cling tightly to proteins like some other drugs do. Only about 30% binds to plasma proteins, meaning the rest floats freely and is ready to act on your heart and blood vessels. This low protein binding reduces the chance of drug interactions. For example, if you’re also taking warfarin or NSAIDs, bisoprolol is less likely to interfere because it’s not competing for the same binding sites.
It also spreads evenly across tissues. Its volume of distribution is around 3.5 L/kg, which means it reaches the heart, kidneys, lungs, and other organs effectively. That’s important because bisoprolol works by blocking beta-1 receptors in the heart - the ones that speed up your heartbeat and raise blood pressure. It doesn’t block beta-2 receptors in the lungs as much as older beta-blockers do, which is why it’s safer for people with asthma or COPD.
How Your Body Breaks Down Bisoprolol
This is where bisoprolol really stands out. Most beta-blockers are broken down by the liver using enzymes like CYP2D6. That creates problems. Some people are fast metabolizers, others are slow - and that leads to wildly different drug levels in the blood. But bisoprolol? Only about 50% of it is metabolized by the liver. The other half leaves the body unchanged through the kidneys.
This dual elimination pathway is a major advantage. Even if someone has liver disease, their bisoprolol levels won’t spike dangerously. The kidneys pick up the slack. Conversely, if someone has kidney problems, the liver still handles half the load. That’s why bisoprolol is often the go-to beta-blocker for elderly patients or those with mixed organ issues.
The main liver enzyme involved is CYP3A4, not CYP2D6. That’s good news because CYP3A4 is less variable between individuals. It’s also less affected by common medications like statins, antibiotics, or antifungals. So, if you’re on multiple drugs, bisoprolol is less likely to interact badly compared to metoprolol or carvedilol.
How Long Bisoprolol Lasts in Your Body
The half-life of bisoprolol is about 10 to 12 hours. That’s longer than metoprolol (3-7 hours) but shorter than atenolol (6-9 hours). Why does this matter? Because a longer half-life means the drug stays active in your system longer, giving you steady, around-the-clock control of your heart rate and blood pressure. That’s why one daily dose is usually enough.
Even though it lasts 10-12 hours, its effects on heart rate and blood pressure can last up to 24 hours. That’s because bisoprolol binds tightly to beta-1 receptors in the heart. Once it attaches, it stays there for a while, even after blood levels start to drop. This receptor-binding behavior is one reason why it’s so effective at low doses - 2.5 mg to 5 mg daily is often enough for most people.
How Age, Kidney Function, and Liver Health Affect Bisoprolol
Age doesn’t change how bisoprolol works in a major way. Older adults clear it slightly slower - mainly because kidney function declines with age - but the change is predictable. Doctors don’t usually need to adjust the dose for age alone. What they do watch is kidney function.
If your creatinine clearance is below 40 mL/min, your doctor will likely lower your dose. That’s because the kidneys handle half the drug. If they’re not working well, bisoprolol can build up. In severe kidney disease, doses may be cut to 2.5 mg daily or even every other day.
Liver disease has less impact. Even in patients with mild to moderate cirrhosis, bisoprolol levels don’t rise dramatically. That’s not true for propranolol or metoprolol, which can become toxic in liver failure. That’s why bisoprolol is often preferred in patients with heart failure and liver problems - a common combo.
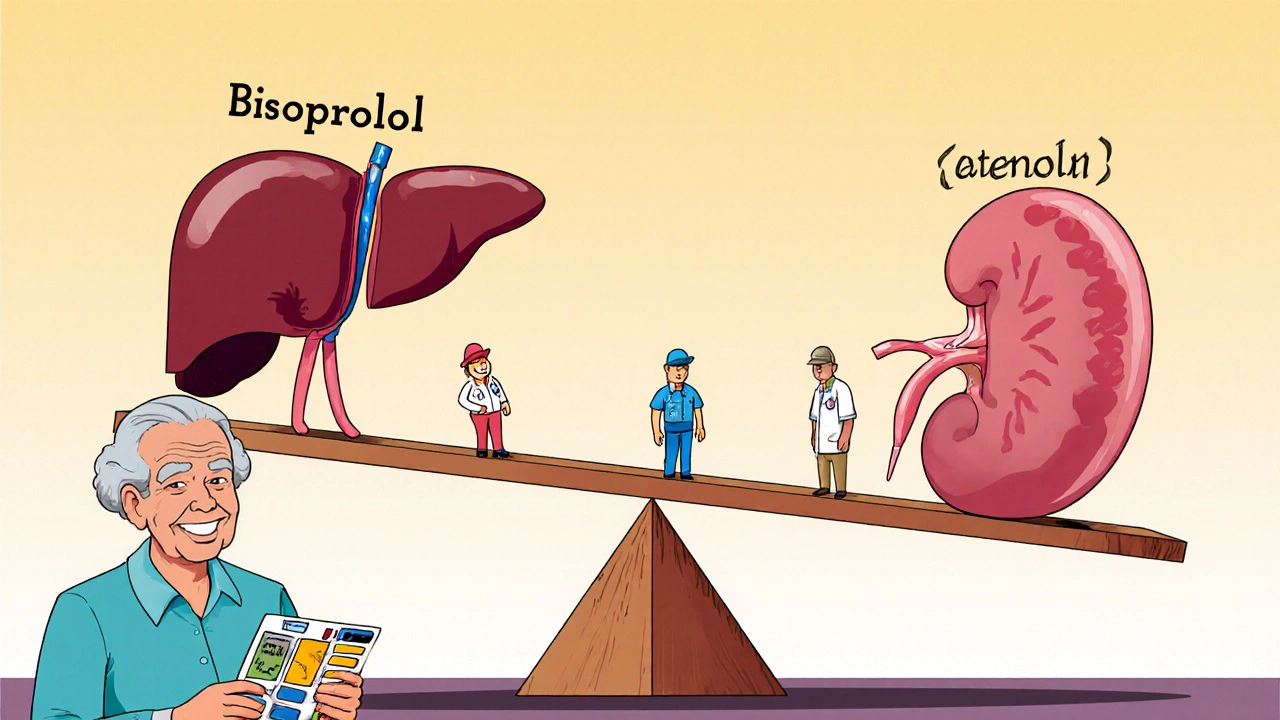
How Bisoprolol Compares to Other Beta-Blockers
Here’s how bisoprolol stacks up against three other common beta-blockers:
| Drug | Absorption (%) | Protein Binding (%) | Primary Elimination Pathway | Half-Life (hours) | Dose Adjustments Needed for Kidney Disease? |
|---|---|---|---|---|---|
| Bisoprolol | 90% | 30% | 50% liver, 50% kidney | 10-12 | Yes, if CrCl < 40 mL/min |
| Metoprolol | 50% | 12% | 95% liver (CYP2D6) | 3-7 | No |
| Atenolol | 50% | 10% | 85% kidney | 6-9 | Yes, if CrCl < 35 mL/min |
| Carvedilol | 65% | 95% | 95% liver (CYP2D6, CYP3A4) | 6-10 | No |
Notice the differences. Bisoprolol has the highest absorption and the most balanced elimination. Metoprolol and carvedilol are heavily liver-dependent, which makes them risky if you have liver damage. Atenolol is mostly kidney-dependent - so if your kidneys fail, it can accumulate fast. Bisoprolol’s middle-ground approach makes it the most forgiving across different patient profiles.
Why This Matters for Real Patients
Let’s say you’re a 72-year-old with high blood pressure and mild kidney decline. Your doctor doesn’t want to risk a drug that could build up and cause your heart to slow too much. Bisoprolol is ideal because even with reduced kidney function, you can still take 2.5 mg or 5 mg safely. You won’t need to split doses or take it twice a day.
Or imagine you’re on statins, antibiotics, or even over-the-counter supplements like St. John’s wort. Bisoprolol won’t react badly with most of them. That’s not true for metoprolol, which can have dangerous interactions with CYP2D6 inhibitors like fluoxetine or quinidine.
And if you’re someone who forgets to take pills - which is common in older adults - bisoprolol’s 24-hour effect means missing a dose by a few hours won’t cause your blood pressure to spike. That’s not true for drugs with shorter half-lives.
What Happens When You Stop Taking It?
You never stop bisoprolol suddenly. Like all beta-blockers, abrupt discontinuation can cause rebound high blood pressure, fast heart rate, or even chest pain. This is because your body has adapted to having the drug around. When it’s gone, your heart’s beta receptors become extra sensitive.
The withdrawal risk is lower with bisoprolol than with propranolol, but it’s still real. If you need to stop - maybe because of side effects or surgery - your doctor will taper the dose over 1-2 weeks. Never cut it on your own.
Final Thoughts: Why Pharmacokinetics Matter
Pharmacokinetics isn’t just for pharmacologists. It’s the reason your doctor picked bisoprolol instead of another beta-blocker. It’s why you can take it once a day. Why it’s safe if you have kidney trouble. Why it doesn’t clash with your other meds. Understanding this isn’t about memorizing numbers - it’s about knowing why your treatment works, and why it’s the right fit for you.
If you’ve ever wondered why your doctor chose bisoprolol over other options, now you know. It’s not random. It’s science - carefully designed to fit real people with real health challenges.
Is bisoprolol safe for people with kidney disease?
Yes, bisoprolol is one of the safest beta-blockers for people with mild to moderate kidney disease because half of it is cleared by the liver. If your kidney function is severely reduced (creatinine clearance below 40 mL/min), your doctor will lower your dose, often to 2.5 mg daily. It’s still safer than drugs like atenolol, which rely almost entirely on kidney clearance.
Can I take bisoprolol with other heart medications?
Bisoprolol has fewer drug interactions than most beta-blockers. It’s generally safe with ACE inhibitors, diuretics, and statins. Because it’s not primarily metabolized by CYP2D6, it doesn’t interact badly with antidepressants like fluoxetine or antifungals like ketoconazole. Still, always tell your doctor about every medication and supplement you take.
Does bisoprolol cause weight gain?
Weight gain is less common with bisoprolol than with older beta-blockers like propranolol. Some patients report a slight increase in weight, but this is usually due to fluid retention or reduced metabolism from slower heart rate - not fat gain. If you notice sudden swelling or unexplained weight gain, talk to your doctor.
How long does it take for bisoprolol to start working?
You may notice a drop in heart rate within 1-2 hours after taking a dose. Blood pressure usually starts to fall within 2-4 hours. But it takes about 1-2 weeks of daily use for the full effect on blood pressure to show. Don’t stop or change your dose if you don’t feel immediate results.
Can bisoprolol cause fatigue or dizziness?
Yes, fatigue and dizziness are common side effects, especially when you first start or increase the dose. This happens because your heart rate slows down. These effects usually improve within a few weeks as your body adjusts. If they’re severe or last longer than a month, your doctor may lower your dose.
Is bisoprolol better than metoprolol for heart failure?
Clinical trials show bisoprolol and metoprolol succinate are equally effective for heart failure. But bisoprolol has a more consistent effect due to its balanced elimination and longer half-life. It’s often preferred because it requires once-daily dosing and has fewer interactions. Metoprolol tartrate, which is taken twice daily, is less predictable.
14 Comments
Niki Tiki
Finally someone explains this without the medical jargon nonsense. Bisoprolol is just smarter than the old junk. My grandpa’s on it and he’s still hiking. Stop prescribing metoprolol like it’s 1995.
Jim Allen
I mean... it’s just a beta-blocker 😴 But yeah, I guess the 50/50 liver-kidney thing is kinda cool. Like nature’s backup system. 🤷♂️
krishna raut
Bisoprolol is ideal for Indian patients with hypertension and mild CKD. Dose 2.5 mg daily if CrCl < 40. Safe, cheap, effective.
Prakash pawar
You know what this really shows? That modern medicine is finally realizing humans aren’t lab rats. We don’t all have perfect livers and kidneys. Bisoprolol is the first beta-blocker that respects our messy biology. We’re not machines bro.
Kathy Pilkinton
I’m glad you mentioned the withdrawal risk. I had a friend who stopped bisoprolol cold turkey after a bad reaction and ended up in the ER with a heart rate of 140. Don’t be that person.
Carolyn Kiger
This is exactly the kind of info I wish my doctor had given me when I was first prescribed this. I’ve been on it for 3 years and never knew why it was chosen over others. Now I feel like I actually understand my own treatment.
Holly Dorger
I’m not a doctor but I’ve been on bisoprolol for 5 years and I swear by it. I used to take metoprolol and felt like a zombie. This one? I still go for runs. And I never have to remember to take it twice a day. Life changer.
Amanda Nicolson
Okay so imagine your body is a city and drugs are delivery trucks. Most beta-blockers? One delivery route only. If the highway’s blocked (liver or kidney fails) everything piles up and there’s a traffic jam. But bisoprolol? Two delivery routes. One goes through the downtown highway, the other takes the scenic backroads. Even if one’s under construction, the meds still get delivered. That’s genius. I’m not a scientist but I watched a lot of YouTube videos about this and now I’m obsessed.
Jackson Olsen
So if you got kidney issues you can still take it? That’s cool. My uncle’s on dialysis and they gave him this instead of the other stuff. He’s still alive so I guess it works.
Penny Clark
I was scared to take this at first cause I thought it’d make me super tired but honestly after 2 weeks I felt better than ever. Like I could think clearer. Maybe it’s the stable BP? Idk but I’m not gonna stop now 💪
Neil Mason
I’m from Canada and we use this a lot up here too. Especially with our aging population. It’s cheaper than carvedilol and just as good. Why pay more if you don’t have to?
Mike Gordon
I’m a nurse. I’ve seen people on metoprolol crash when their liver fails. Bisoprolol? Not so much. It’s the quiet hero of cardiology. No fanfare. No hype. Just works. And that’s why docs keep prescribing it.
Arrieta Larsen
I’ve been on this for 7 years. Never had side effects. My doctor said it’s because of the dual elimination. I didn’t even know what that meant until I read this. Now I feel smart.
Nate Girard
This is why I love learning about meds. It’s not just about taking a pill-it’s about how your body works. Bisoprolol isn’t magic, it’s science designed for real people. Thank you for writing this. I’m sharing it with my mom who’s on it too.

Write a comment