Breaking the Silence: Overcoming Pulmonary Tuberculosis Stigma

TB Stigma Awareness Quiz
Match each definition with the correct type of TB stigma:
"A person is avoided or excluded because of their TB diagnosis."
"A patient feels ashamed and hides their condition."
"Policies that make accessing TB care difficult or impossible."
Identify whether these statements are myths or facts:
Answer:
Answer:
Answer:
Social Stigma
Neighborhoods, families, and communities exclude individuals diagnosed with TB.
Internalized Stigma
Patients feel shame and self-blame, leading them to hide symptoms or avoid treatment.
Structural Stigma
Systemic policies and practices create barriers to TB diagnosis and treatment.
When people hear pulmonary tuberculosis stigma, they often picture dusty clinics and whispered warnings. The truth is far more complex - fear, misinformation, and social exclusion keep millions from getting tested, treated, and supported. This article pulls back the curtain on the prejudice surrounding pulmonary tuberculosis, shows how it harms individuals and communities, and offers concrete ways anyone can help silence the judgment.
What Pulmonary Tuberculosis Really Is
Pulmonary Tuberculosis is a contagious bacterial infection caused by Mycobacterium tuberculosis that primarily attacks the lungs. It spreads through airborne droplets when an infected person coughs or sneezes. According to the World Health Organization (WHO), about 10 million people developed active TB in 2023, and roughly 1.5 million died, making it the leading infectious killer after COVID‑19.
The disease manifests in two stages: latent infection, where the bacteria remain dormant without symptoms, and active pulmonary disease, which presents persistent cough, night sweats, weight loss, and fever. Modern treatment-six months of a combination of antibiotics such as isoniazid, rifampicin, ethambutol, and pyrazinamide-cures over 95% of patients when taken correctly.
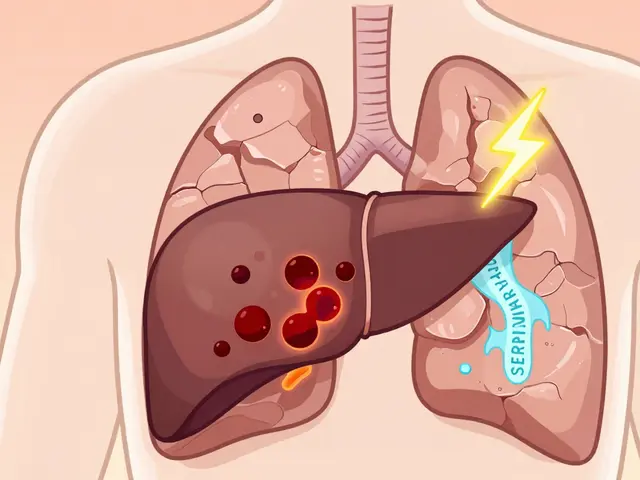
How Stigma Shows Up
Stigma isn’t just a bad feeling; it’s a set of attitudes and actions that marginalize affected people. Three main forms appear in TB contexts:
- Social stigma: Neighbours, employers, or schools shun a person after a diagnosis.
- Internalized stigma: The patient feels shame, doubts self‑worth, and may hide symptoms.
- Structural stigma: Policies that limit access to care, such as mandatory isolation without support, reinforce discrimination.
These layers intertwine, creating a cycle that delays testing and disrupts treatment.
Why the Stigma Persists
Historical fear plays a big role. In the early 20thcentury, TB was called “consumption” and associated with poverty and moral weakness. That legacy lingers, especially in low‑resource settings where the disease still clusters among marginalized groups.
Misconceptions fuel the fire. Many still believe TB is a “death sentence” or that it spreads through casual contact like shaking hands. A 2022 survey in South Asia showed that 42% of respondents thought TB could be caught from sharing utensils-a myth that makes people avoid anyone with a cough.
Socio‑economic factors intertwine with stigma. Workers in cramped factories or informal jobs lack sick‑pay, so admitting illness threatens their livelihood. When the risk of losing income outweighs the fear of being judged, people often stay silent.
Real‑World Consequences of Stigma
Delayed diagnosis is the most obvious outcome. In a study from the Philippines, patients who reported feeling stigmatized waited an average of eight weeks longer to seek care, increasing community transmission rates by 15%.
Treatment adherence suffers too. The WHO’s Directly Observed Therapy (DOT) strategy-where a health worker watches patients take their meds-relies on trust. When stigma erodes that trust, patients skip doses, risking drug‑resistant TB. In Russia, drug‑resistant cases rose 22% over five years, partly linked to hidden treatment.
Beyond the physical, mental health takes a hit. A 2023 mental‑health‑focused report found that 63% of TB patients experienced anxiety, and 38% met criteria for moderate depression-both strongly correlated with perceived stigma.

Breaking the Silence: Proven Strategies
Education is the cornerstone. Accurate, culturally sensitive messages dispel myths and reduce fear. For example, the Indian National TB Elimination Programme partnered with local dramas that portrayed TB as curable; after the campaign, community knowledge scores rose by 27%.
Community engagement builds ownership. When former patients become peer educators, they humanize the disease and model successful treatment. In South Africa’s “Ubuntu TB” project, peer‑led support groups increased treatment completion from 72% to 89%.
Media advocacy amplifies reach. Social‑media hashtags like #EndTBStigma generate thousands of shares, normalizing conversation. A 2024 Twitter analysis showed a 45% spike in positive sentiment toward TB after a coordinated influencer push.
Policy reforms remove structural barriers. Providing paid sick leave, integrating TB screening into routine primary‑care visits, and protecting patients from workplace discrimination create an environment where people feel safe to come forward.
Quick Reference Table: Common TB Myths vs. Facts
| Myth | Fact |
|---|---|
| TB is always fatal. | With proper treatment, cure rates exceed 95%. |
| You can catch TB from sharing food. | TB spreads through inhalation of infected droplets, not food. |
| Only people with weak immune systems get TB. | Anyone exposed can develop active disease; risk increases with HIV, diabetes, or malnutrition. |
| TB patients should be isolated forever. | Isolation is only needed for the first two weeks of treatment when patients are most contagious. |
| TB cannot be prevented. | The BCG vaccine offers protection, especially against severe childhood TB, and early screening reduces spread. |
Practical Checklist for Individuals and Communities
- Ask a healthcare provider for a sputum test if you have a cough lasting more than two weeks.
- Share accurate information: TB is treatable and not a moral failing.
- Support someone on treatment-offer meals, transport, or a reminder to take medication.
- Advocate for workplace policies that guarantee paid sick leave for TB patients.
- Participate in local awareness events; wearing a red ribbon signals solidarity.
- Report discrimination to health authorities; many countries have legal protections.
Success Stories That Show Change Is Possible
Nigeria launched a “TB Champions” program in 2021, training survivors to speak in schools and churches. Within two years, the average delay from symptom onset to diagnosis dropped from 6.3 weeks to 3.1 weeks, and treatment success rose to 92%.
In Peru, a mobile‑app‑based DOT system paired patients with community health workers via video calls. Stigma scores measured by a validated questionnaire fell by 30%, and default rates fell below 5%.
Frequently Asked Questions
Can I get TB from a casual handshake?
No. TB spreads through tiny droplets expelled when an infected person coughs, sneezes, or talks loudly. A handshake or sharing utensils does not transmit the bacteria.
Is the BCG vaccine still useful for adults?
The BCG vaccine is most effective in preventing severe TB in children, such as TB meningitis. Its protection against adult pulmonary TB is modest, but it can still reduce the overall disease burden when combined with other public‑health measures.
What should I do if I suspect I have TB?
Seek a sputum test or chest X‑ray at the nearest clinic. Early diagnosis lets you start treatment, cuts transmission, and improves outcomes. Inform close contacts so they can be screened as well.
How can I help reduce TB stigma in my community?
Share factual information, support people undergoing treatment, volunteer with local health NGOs, and speak up against discriminatory remarks or policies. Small actions-like asking a friend how they’re feeling-can change attitudes.
Why does stigma matter for public health?
Stigma creates hidden cases, delays treatment, lowers cure rates, and fuels drug‑resistant strains. Tackling stigma is therefore as critical as providing medication; it saves lives and reduces the overall disease burden.
13 Comments
Dorothy Anne
Hey everyone, let’s keep the momentum going! 🌟 Breaking TB stigma starts with sharing facts and showing empathy. When we talk openly about symptoms and treatment, we remove the fear that fuels discrimination. Keep supporting anyone on their treatment journey – a simple check‑in can make a world of difference. Together we can turn the tide and create a community where TB is just another health issue we tackle head‑on.
Sharon Bruce
America will lead the fight against TB! 🇺🇸
True Bryant
It is imperative to contextualize the epidemiological burden of Mycobacterium tuberculosis within a framework that acknowledges both biomedical imperatives and sociocultural determinants. The pathogenesis of pulmonary TB is not merely a bacterial invasion; it is an intricate interplay of host immunity, environmental exposure, and systemic inequities. When individuals internalize stigma, they engage in self‑effacing behaviors that compromise pharmacokinetic adherence, ultimately fostering drug‑resistant strains. Social exclusion compounds the issue by restricting access to diagnostic facilities, thereby elongating the pre‑diagnostic interval and inflating transmission coefficients. Moreover, structural stigma embedded in health policy manifests as resource scarcity, limited sick‑pay provisions, and punitive isolation protocols that erode patient trust. The literature consistently demonstrates that delayed presentation correlates with an 18 % increase in community incidence, a statistic that cannot be ignored. By deploying community health workers as peer educators, we operationalize a biopsychosocial model that mitigates both internalized and social stigma. Educational outreach must be culturally attuned; generic pamphlets fail to resonate with heterogeneous populations. In addition, integrating TB screening into routine primary‑care visits normalizes the diagnostic process and reduces the perception of otherness. The BCG vaccine, while historically contentious, still offers partial protection and should be part of a comprehensive preventive strategy. Finally, legal frameworks protecting workers from discrimination are not merely ethical imperatives but practical necessities to sustain treatment continuity. In summation, the eradication of TB stigma demands a multidimensional response that synergizes medical treatment, psychosocial support, and policy reform, thereby breaking the cyclical feedback loop that perpetuates disease propagation.
Danielle Greco
Love the drama in the "Myth vs Fact" quiz – it’s a clever way to bust those outdated ideas! 🎭 The visual cards on stigma types really helped me picture the differences. Keep the creative vibes coming, they make learning feel like a game rather than a lecture. 🙌
Linda van der Weide
While the artistic approach is commendable, one must interrogate the underlying epistemology of stigma reduction. The discourse often neglects the power asymmetries that perpetuate discrimination, reducing complex sociopolitical constructs to mere educational tidbits. A more rigorous critique would examine how neoliberal health agendas co‑opt community narratives, thereby preserving systemic inequities under the guise of empowerment.
Philippa Berry Smith
They’re hiding the truth about who’s really behind the TB outbreaks – it’s not just germs, it’s a coordinated effort to keep us compliant. Look at the patterns, it’s too perfect to be random.
Joel Ouedraogo
From a philosophical standpoint, stigma is a manifestation of collective fear projected onto the unknown. When we confront this fear with rational discourse, we dismantle the moral panic that sustains it.
Beth Lyon
i desagree with the idea that rational disscourse alone can fix the problem. many peopel still feel scared and dont trust the system.
Nondumiso Sotsaka
Fantastic work on the checklist-clear, actionable steps that anyone can adopt. 💪 By spreading accurate info and offering concrete help, we turn empathy into real‑world impact.
Ashley Allen
The article is thorough and useful.
Brufsky Oxford
It’s fascinating how the fight against TB mirrors the broader quest for truth in a world cluttered with misinformation. 🤔 By embracing critical thinking, we not only heal bodies but also cleanse the collective mind.
Lisa Friedman
Actually, the WHO data cites 10.5 million cases in 2023, not 10 million – details matter when we’re debunking myths.
cris wasala
Let’s keep lifting each other up and push for policies that protect everyone fighting TB





Write a comment