Graft Failure: Causes, Risks, and How to Manage Them
When talking about Graft Failure, the loss of function in a transplanted organ or tissue due to complications after surgery. Also known as transplant failure, it can happen in kidney, heart, liver, or bone‑marrow transplants and often signals a deeper problem that needs immediate attention. Understanding why it occurs helps you catch warning signs early and act before permanent damage sets in. graft failure isn’t just a medical buzzword; it’s a real risk that affects patient survival and quality of life.
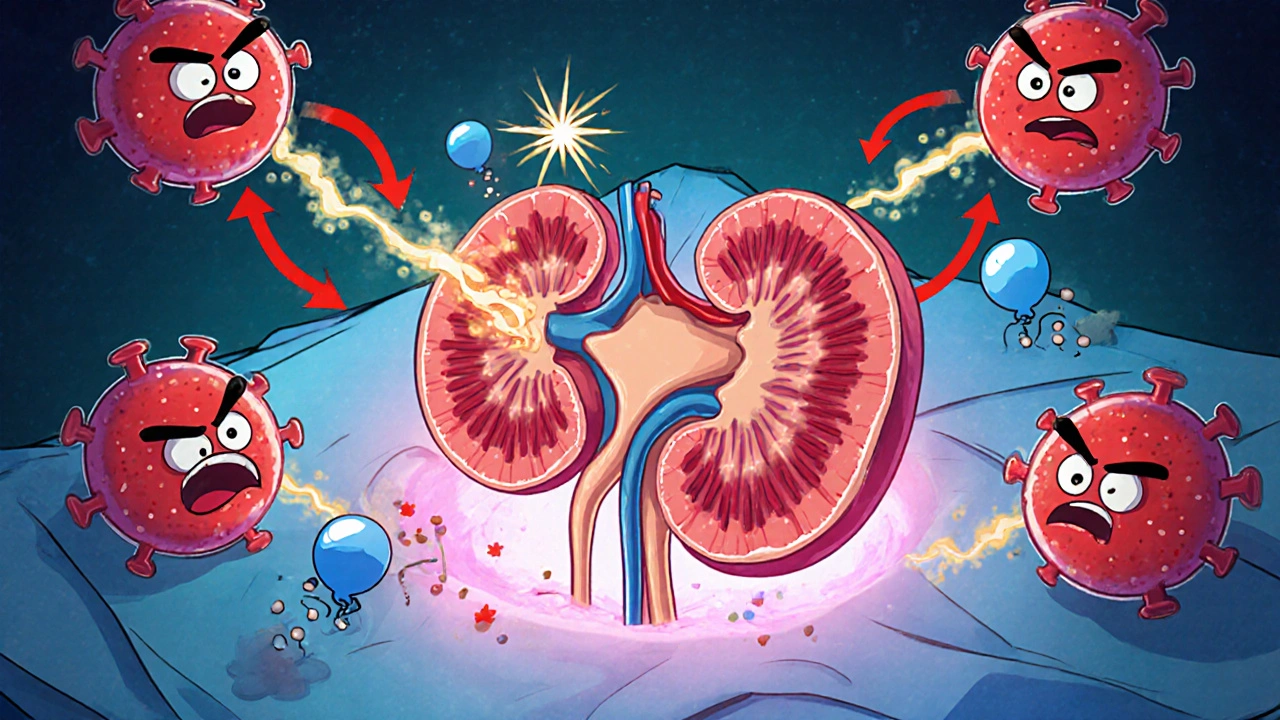
Most graft failures stem from three big culprits: the body’s immune attack, poor blood flow, and infection. Transplant Rejection, an immune‑mediated response where the recipient’s system attacks the donor tissue is the classic cause and can be acute or chronic. When rejection isn’t controlled, the graft’s blood vessels can narrow, leading to Ischemia, insufficient oxygen delivery to the transplanted organ due to reduced blood flow. Ischemia not only damages cells but also creates a fertile ground for bacterial or viral infections, which add another layer of risk. Together, these factors create a vicious cycle that can seal the fate of the graft.
Key Factors that Influence Graft Survival
Managing graft failure starts with the right Immunosuppressive Therapy, a regimen of drugs designed to dampen the immune response and prevent rejection. Choosing the correct mix—often a calcineurin inhibitor, an antiproliferative agent, and corticosteroids—depends on the organ type, patient age, and comorbidities like diabetes or hypertension. Over‑suppression can invite infections, while under‑suppression leaves the door open for rejection. Recent studies show that tailoring doses based on blood‑level monitoring reduces both rejection and infection rates, a balance highlighted in many of our drug comparison articles.
Even with perfect medication, you need vigilant monitoring. Regular blood tests, imaging studies, and biopsy when needed keep you ahead of trouble. If ischemia is spotted early, interventions like re‑vascularization or, in rare cases, localized removal of damaged tissue can save the graft. One emerging salvage option is Cryoablation, the use of extreme cold to destroy problematic tissue while preserving surrounding structures. Although primarily used for tumors, cryoablation is being explored to treat focal graft lesions that don’t respond to medication, offering a minimally invasive route to prolong graft function.
Beyond meds and procedures, lifestyle plays a silent but powerful role. Staying hydrated, maintaining a balanced diet rich in antioxidants, and avoiding smoking help keep blood vessels healthy and reduce the strain on the transplanted organ. Patient education—knowing the signs of rejection (fever, pain, swelling) and ischemia (sudden loss of organ function)—empowers quick action. Our collection below dives deep into these topics: from detailed drug comparisons for immunosuppression, to guides on managing heart rhythm issues in diabetic patients, and practical tips on using inhalers or coping with infection risks. Scan the articles to arm yourself with the exact knowledge you need to protect your graft and improve long‑term outcomes.
Understanding How Organ Rejection Leads to Post-Transplant Complications
Explore how organ rejection sparks post‑transplant complications, learn the types, risk factors, monitoring tools, and management strategies to protect graft health.
Read More