Melphalan: What It Is and How It’s Used
Melphalan is a chemotherapy drug doctors use to treat cancers like multiple myeloma and ovarian cancer. It’s an alkylating agent — that means it damages DNA in fast-growing cells so the tumor can’t keep dividing. That’s why it works, and why normal cells get hit too.
You’ll see melphalan given by mouth or through a vein. In high doses it’s used before a stem cell transplant to wipe out bone marrow, then healthy stem cells are returned. Lower doses are used for maintenance or to control symptoms.
What to expect while taking melphalan
Common side effects include low blood counts, which raise infection and bleeding risks. Expect fatigue, nausea, and mouth sores. Some people notice hair thinning. Your team will check blood counts often and may delay treatment if levels drop too low.
Fertility can be affected — sperm and egg production may fall after treatment. If you might want children later, talk to your doctor about sperm banking or other options before starting melphalan.
Take anti-nausea meds if prescribed. For mouth sores, keep up gentle oral care and tell your nurse early about any pain or white patches. If you get a fever, call your clinic right away — low counts plus fever is treated as an emergency.
Practical tips, interactions, and safety
Melphalan can interact with other drugs that suppress bone marrow or increase bleeding risk. Always give the full med list to your oncology team — that includes over-the-counter pain relief, herbal supplements, and vitamins. Some vaccines (live vaccines) may be unsafe while your immune system is down.
Handling precautions matter: people giving or preparing melphalan follow strict safety rules to avoid exposure. If you handle pills at home, wash your hands after touching them and avoid crushing tablets unless instructed. Store melphalan as your clinic tells you — usually away from heat and moisture.
If you have kidney or liver problems, dose adjustments are common. Your doctor will tailor the dose based on labs and overall health. The goal is to balance effect on the cancer with the side effects you can safely manage.
Questions to ask your team: How long will treatment last? What specific side effects should I watch for? Will I need growth factors or transfusions? Should I avoid certain foods, alcohol, or other medicines? Ask for written instructions on handling and emergency contacts.
Typical oral doses vary: low-dose regimens might be 2 to 8 mg daily for several days, while high-dose conditioning can total hundreds of mg given over a few days in hospital. Exact dosing depends on body size, kidney function, and treatment goal. Pregnant people should not take melphalan — it can cause birth defects. If you're breastfeeding, stop and discuss alternatives. Keep a medication diary and bring all questions to each visit. Bring a friend to appointments.
Melphalan can be an effective part of cancer care, but it needs careful monitoring. Keep open communication with your healthcare team, report new symptoms fast, and plan for support during low-blood-count periods. That practical approach helps you get the most benefit while managing risks.
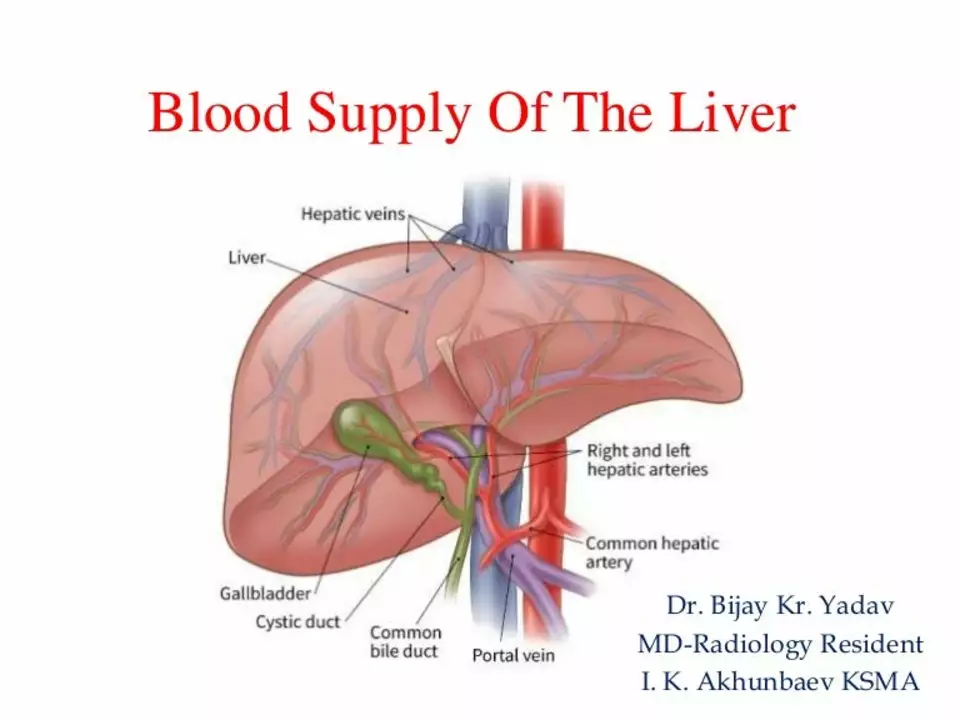
Melphalan and the Liver: Understanding Hepatic Toxicity and Management Strategies
In my recent research, I delved into the effects of Melphalan on the liver, specifically focusing on hepatic toxicity and management strategies. I found that Melphalan, a chemotherapy drug, can cause liver damage in some patients, which is a concerning side effect. However, there are ways to manage and minimize these risks, including monitoring liver function tests and adjusting dosages. Additionally, some studies suggest that using other medications alongside Melphalan may help protect the liver. Overall, it's essential for healthcare providers and patients to be aware of these risks and management strategies to ensure the safe use of Melphalan.
Read More